CASE20230821_005
The Pressure in Imaging: To See or Not to See
By Kristy Garganera, Bryan Rene Toledano, Michelangelo L. Sabas
Presenter
Kristy Brillantes Garganera
Authors
Kristy Garganera1, Bryan Rene Toledano1, Michelangelo L. Sabas1
Affiliation
The Medical City, Philippines1,
View Study Report
CASE20230821_005
Imaging & Physiology - Invasive Imaging (IVUS, OCT, NIRS, VH, etc)
The Pressure in Imaging: To See or Not to See
Kristy Garganera1, Bryan Rene Toledano1, Michelangelo L. Sabas1
The Medical City, Philippines1,
Clinical Information
Relevant Clinical History and Physical Exam
63 year old male HASCVD, diabetic,S/P CABG,S/P PCI for ISR coming in for angina with new wall motion abnormalities in point of care ultrasound at the ER.Patient with 6/10 anterior chest pain,clear breath sounds,good peripheral pulses.BP 110/70, heart rate 98 bpm sinus rhythm. Patient had previous NSTEACS 7 months prior underwent LM bifurcation PCI of the left main using DK crush. 6 months prior came in again for NSTEACS with ostial circumflex lesion underwent PCI using drug coated balloon.
 RAO 7 mos prior NT.avi
RAO 7 mos prior NT.avi
 final angio post pci NT 7 mos prior.avi
final angio post pci NT 7 mos prior.avi
 RCA NT 7 mos prior.avi
RCA NT 7 mos prior.avi
Relevant Test Results Prior to Catheterization
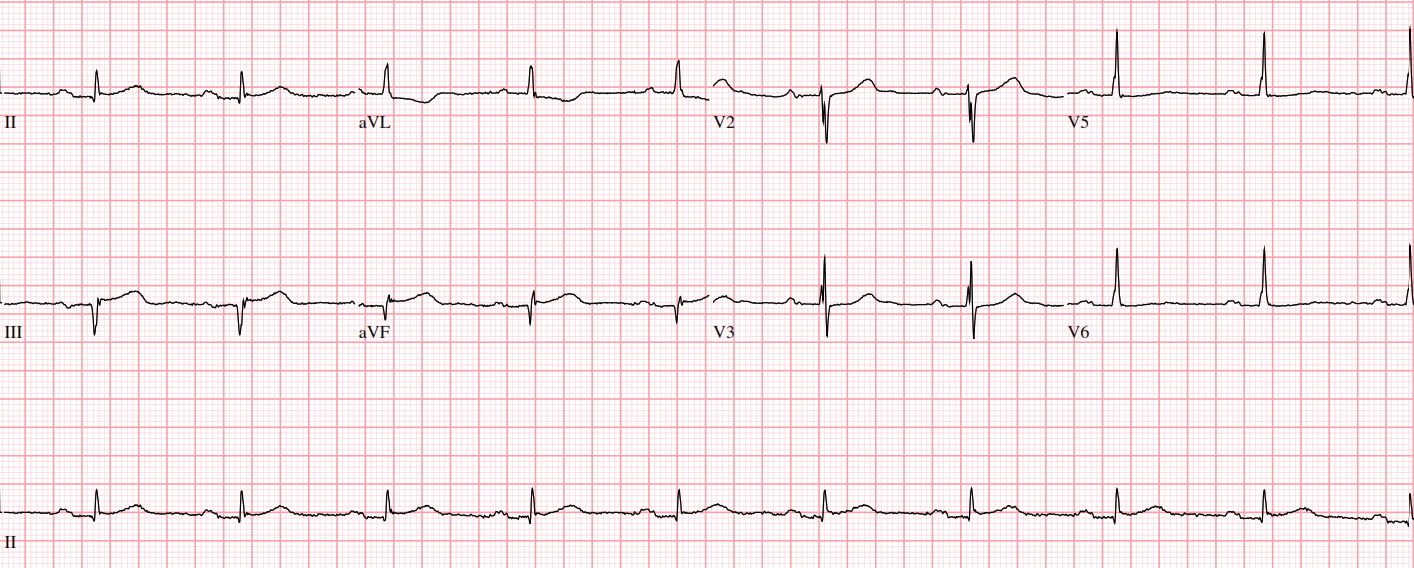
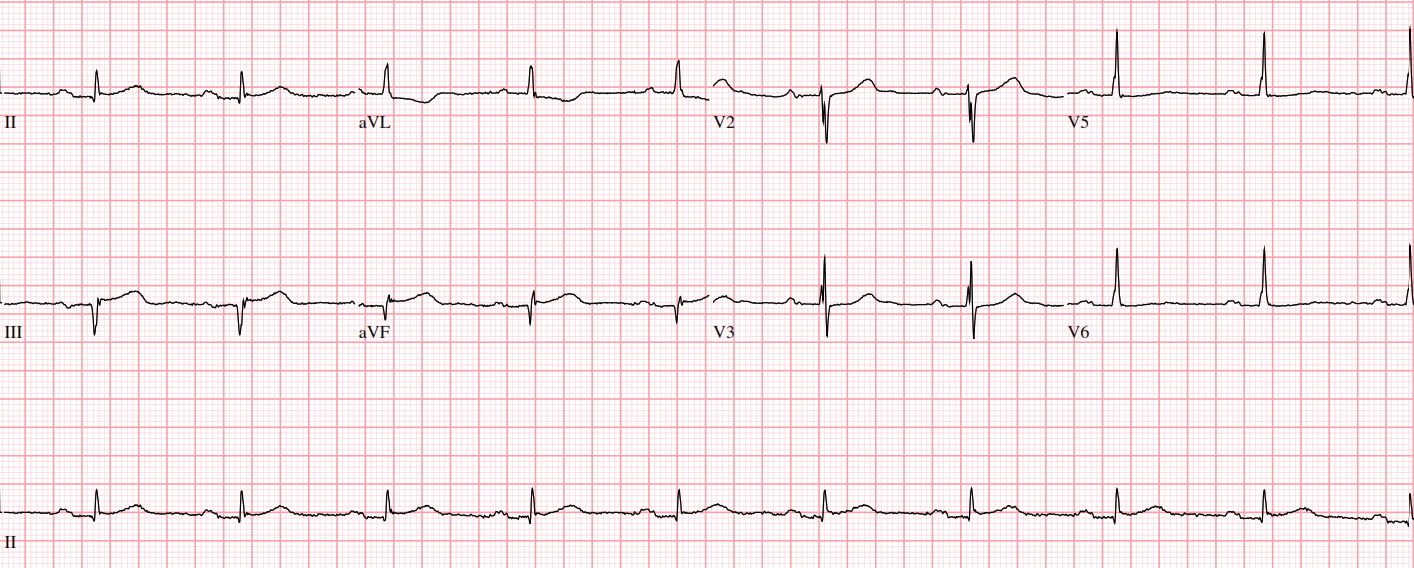
Troponin 0.11ECG: Sinus rhythm, anteroseptal wall ischemia
Relevant Catheterization Findings
Left Main: 4.5 mm vessel with patent stentLeft Anterior Descending Artery: Patent 4.0 mm vessel with patent proximal to mid segment stent, 40% mid segment ISR, 70% distal segment stenosisLeft Circumflex Artery: 3.5 mm vessel with 50-60% ostial segment stenosisRight Coronary Artery: patent proximal to mid segment stent. Chronic Total Occlusion of the mid segment.
 RAO CAUD NT.avi
RAO CAUD NT.avi
 RAO CRAN NT.avi
RAO CRAN NT.avi
 LAO CAUD NT.avi
LAO CAUD NT.avi
Interventional Management
Procedural Step
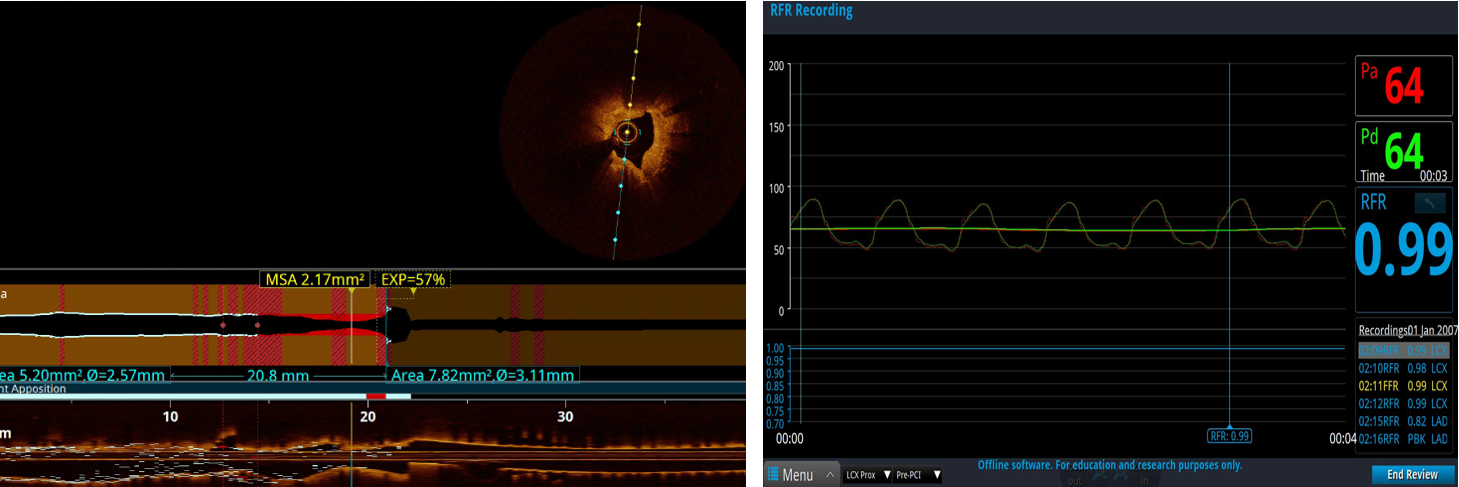
OCT of Left Anterior Descending showed thick layers of fibrous plaque and neoatheroma despite well apposed stent struts with cross-sectional area (CSA) of 2.68mm2 in the distal segment and 2.9mm2 in the mid segmentOCT run of the Left Circumflex showed fibrocalcific plaques with ostial CSA of 2.17mm2PCI of the distal Left Anterior Descending done using a 2.25x18mm stent and postdilated with NC 2.5x12 mm balloon. But post PCI, our resting full-cycle ratio (RFR) showed values of 0.77 in distal, 0.82 in mid with a step up on pullback of 0.89 at the proximal segment. Hence we proceeded by stenting the ambiguous mid segment lesion using a 2.5x10mm and 2.75x33mm stents and postdilated using 3.0x20mm balloon at 19 ATM. But surprisingly, our RFR still showed values of 0.83 and 0.86 with step up to 0.89 at the proximal segment before the proximal stent edge. OCT showed minimal areas of malapposition. We were left to a decision on what else to do, so we further postdilated using an NC 3.0x20mm balloon at 26-30 ATM which finally achieved an RFR value of 0.90.Going back to the Left Circumflex, our ostial CSA showed 2.17 mm2 on OCT but multiple RFR runs showed values of 0.99 and no further intervention was done.
 LCX Prox Pre PCI.mp4
LCX Prox Pre PCI.mp4
 LAD Distal Pre PCI.mp4
LAD Distal Pre PCI.mp4
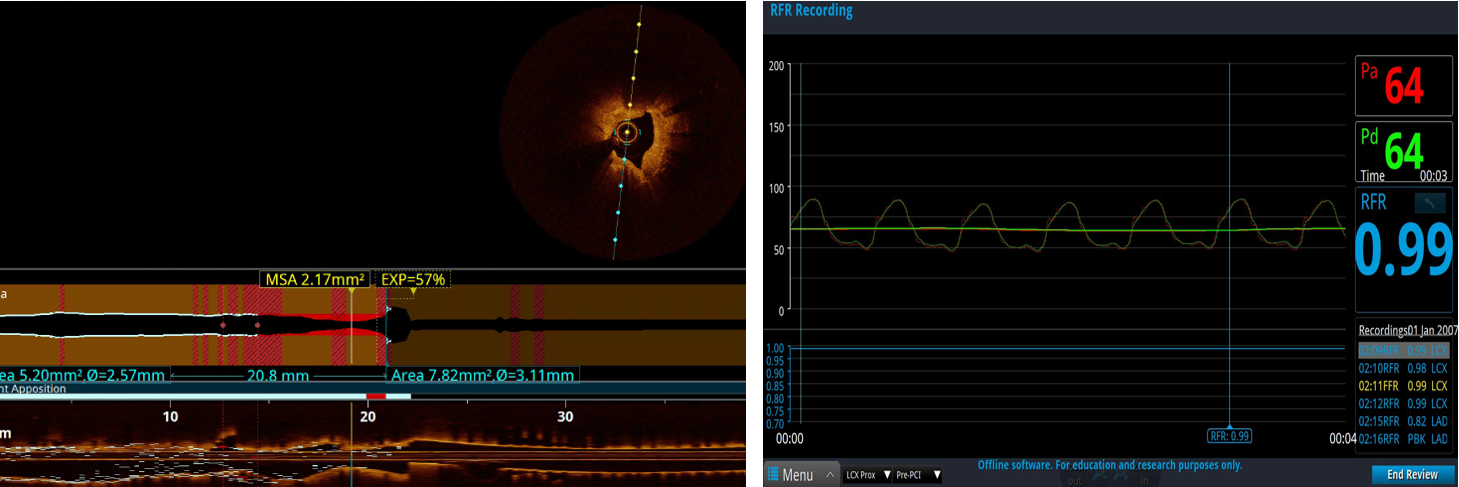
Case Summary
This patient had a bad history of ISR with recent drug coated balloon angioplasty of the ostial LCx but presents with anterior wall hypokinesia on echocardiography. We anticipated to fix the LCx but physiology said otherwise hence saving him from a complex left main intervention. Intravascular Optical Coherence Tomography is a useful tool to assess long and ambiguous lesions and optimize stent implantation especially in the setting of in-stent restenosis. However, as interventional cardiologist, we have the itch to fix what looks tight. In the advent of coronary physiology, we avoid this temptation and give proper adjudication to coronary lesions.
