CASE20230825_026
Absent Left Main Coronary Artery in a 39 Year-Old Filipino Female Presenting as St-Elevation Myocardial Infarction: A Case Report
By Florimond Joseph Martin Garcia Jr.
Presenter
Florimond Joseph Martin Garcia Jr.
Authors
Florimond Joseph Martin Garcia Jr.1
Affiliation
The Medical City, Philippines1,
View Study Report
CASE20230825_026
Complex PCI - Left Main
Absent Left Main Coronary Artery in a 39 Year-Old Filipino Female Presenting as St-Elevation Myocardial Infarction: A Case Report
Florimond Joseph Martin Garcia Jr.1
The Medical City, Philippines1,
Clinical Information
Relevant Clinical History and Physical Exam
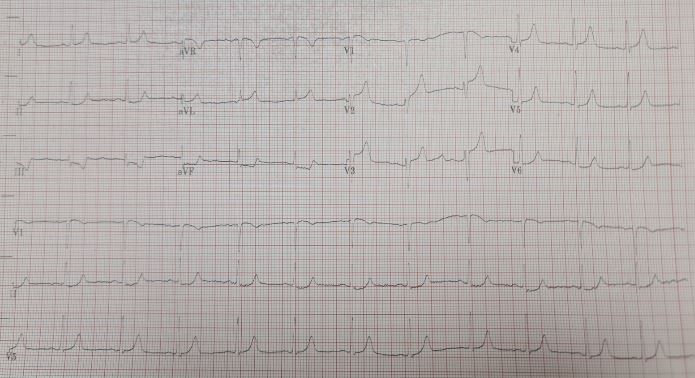
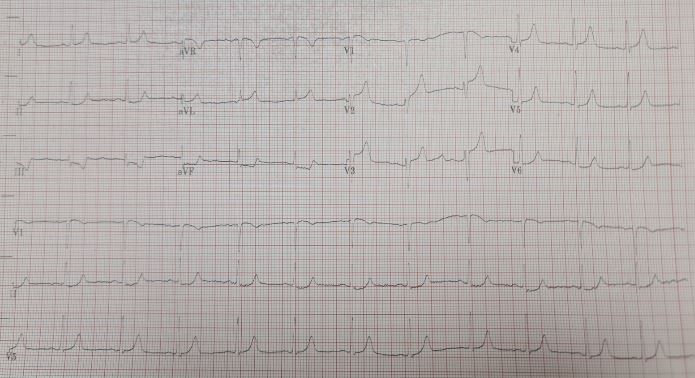
This is a case of a 39 year-old Filipino female, hypertensive, who initially presented with sudden severe chest pain. She then sought emergency consult at our institution with a normal initial 12-lead ECG and high sensitivity troponin I. On the third hour of consult, she went into pulseless ventricular tachycardia. Advanced cardiac life support was performed with return of spontaneous circulation after 5 min. Repeat12-lead ECG showed anterior wall ST elevation. Catheterization lab was activated.


Relevant Test Results Prior to Catheterization
12 Lead ECG: Sinus Rhythm, Normal Axis, Anterior Wall ST elevation.High Sensitivity Troponin I: 7.8 ng/LNT-pro BNP: 134 pg/ml
Relevant Catheterization Findings
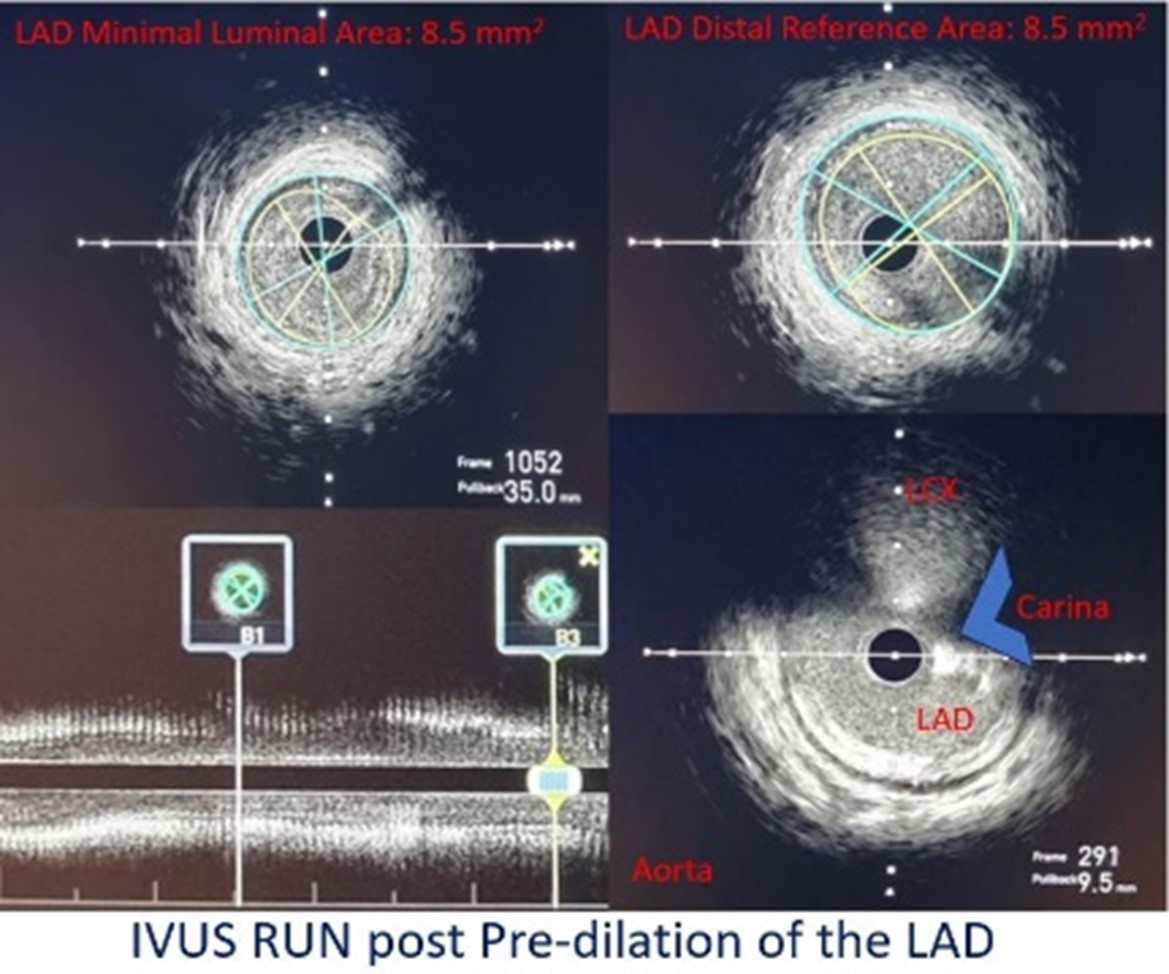
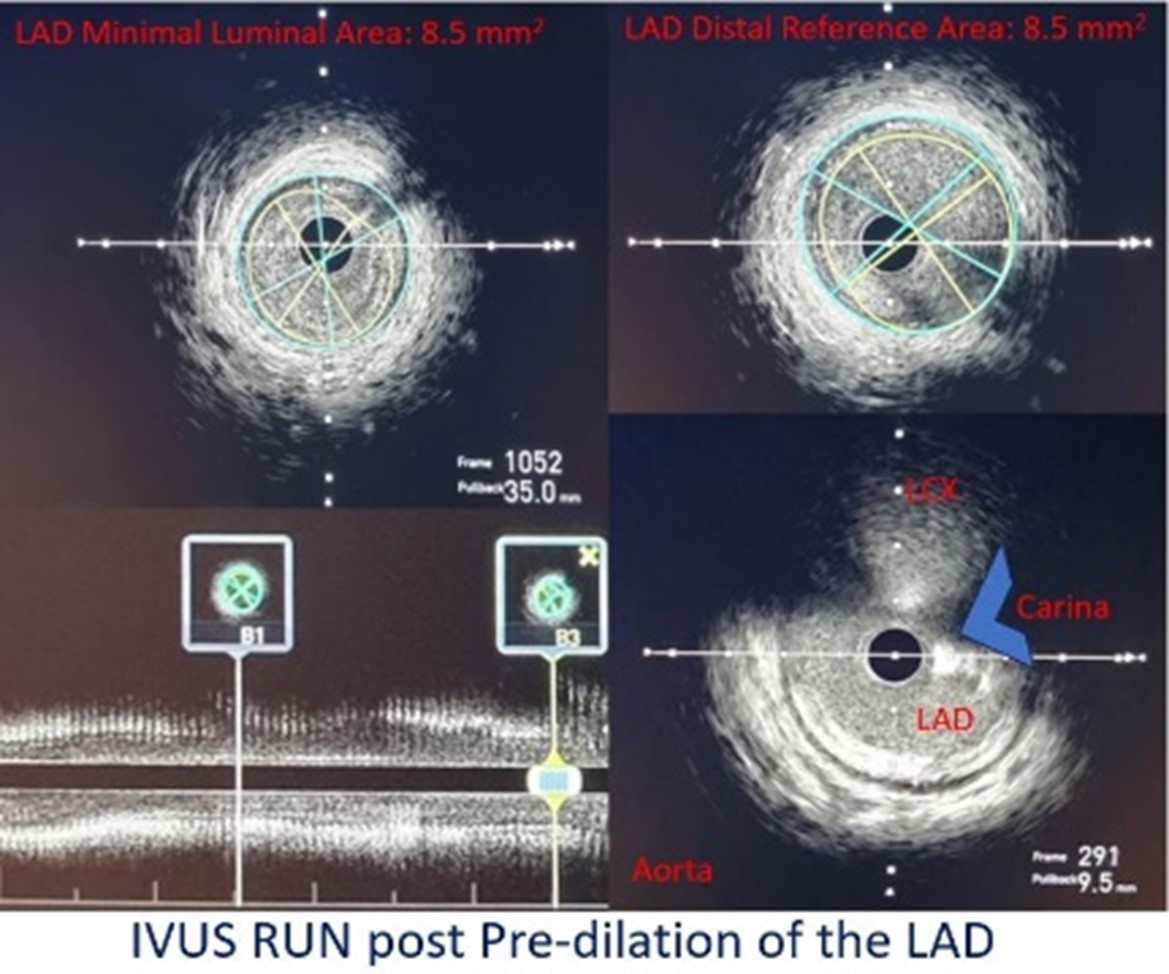
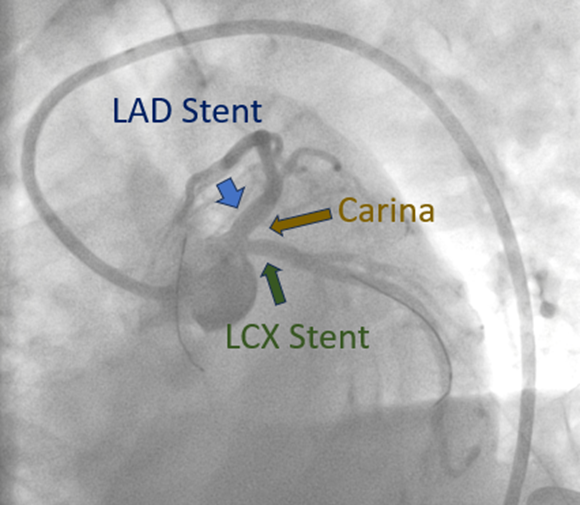
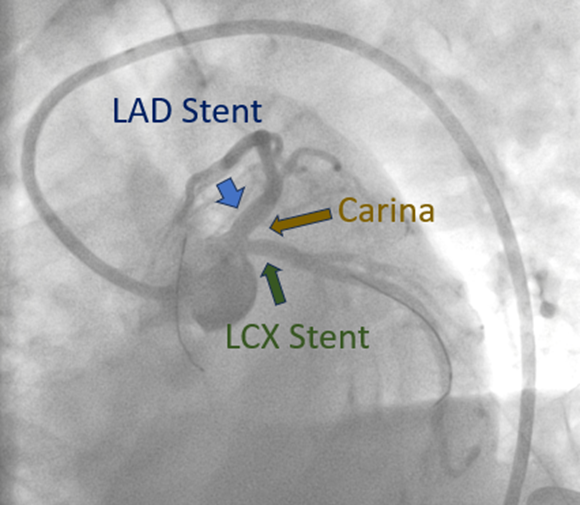
Coronary angiogram revealed an absent left main artery with a 95% ostio-proximal stenosis of the left anterior descending artery (LAD) and an 80% ostio-proximal stenosis of the left circumflex artery (LCX). Intravascular ultrasound (IVUS) of the LAD lesion showed mixed plaque with a distal reference cross-sectional area (CSA) of 8.5 mm2, a minimal luminal CSA of 5.26 mm2 and confirmed an absent left main artery.


Interventional Management
Procedural Step
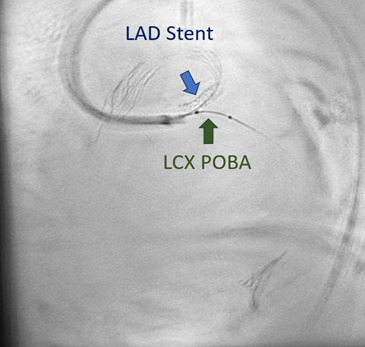
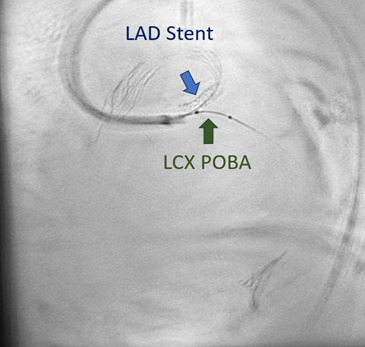
Culprit vessel stenting of the LAD was done using a 3.5 x 15 mm stent, with 2 stent struts exposed at the aortic lumen. IVUS of the LCX showed mixed plaque with a distal reference CSA of 6.01 mm2 and a minimal luminal CSA of 3.4 mm2. Plain old balloon angioplasty of the LCX was done. Post PCI angiogram showed no residual stenosis in the LAD with TIMI III flow but with a residual 90% stenosis in the LCX ostium. Completion stenting of the LCX was deferred due to cardiogenic shock.


Case Summary
In conclusion, congenital anomalous coronary arteries may present with life threatening complications and management of these patients should be individualized depending on the anatomy, condition on presentation, and diagnostic and imaging findings. Decision to do a culprit only versus a complete PCI strategy should be done with the consideration of the patient’s current state, utilizing available tools such as the intravascular ultrasound.
