CASE20250701_001
Management of Distal Coronary Artery Perforation
By Justin Ka-Ho Wong
Presenter
Justin Ka-Ho Wong
Authors
Justin Ka-Ho Wong1
Affiliation
Pamela Youde Nethersole Eastern Hopsital, Hong Kong, China1
View Study Report
CASE20250701_001
Complication Management - Complication Management
Management of Distal Coronary Artery Perforation
Justin Ka-Ho Wong1
Pamela Youde Nethersole Eastern Hopsital, Hong Kong, China1
Clinical Information
Relevant Clinical History and Physical Exam
An 83 year-old female with diabetes, dyslipidaemia, and chronic renal disease presented with worsening angina since January 2025. She had CT coronary angiogram done in February 2023, which showed moderate RCA disease. Her symptoms were well-controlled until early this year and was referred for revascularisation. PCI was performed but complicated with distal wire trauma with perforation. The perforation site was successfully managed by Vicryl embolisation.
Relevant Test Results Prior to Catheterization
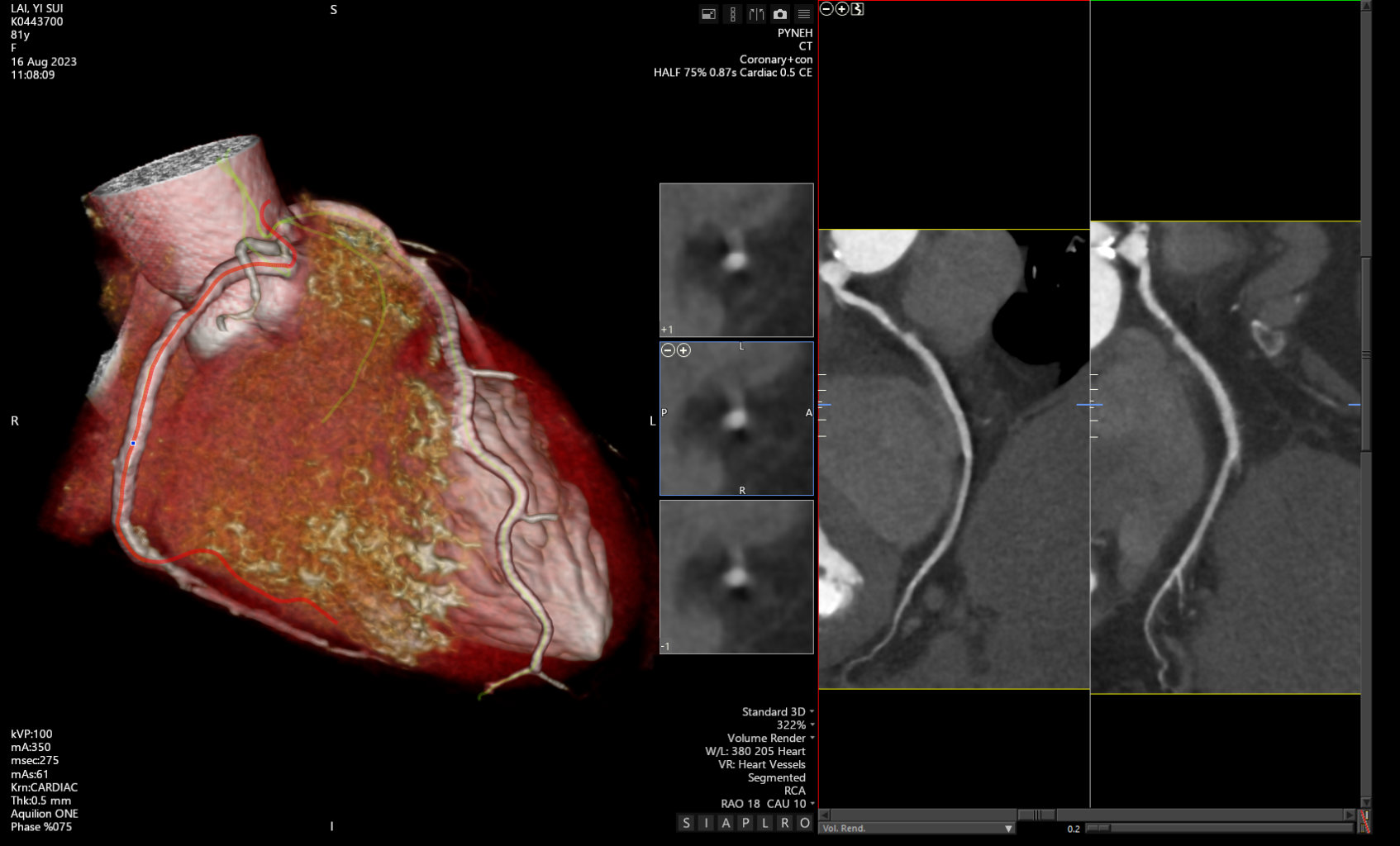
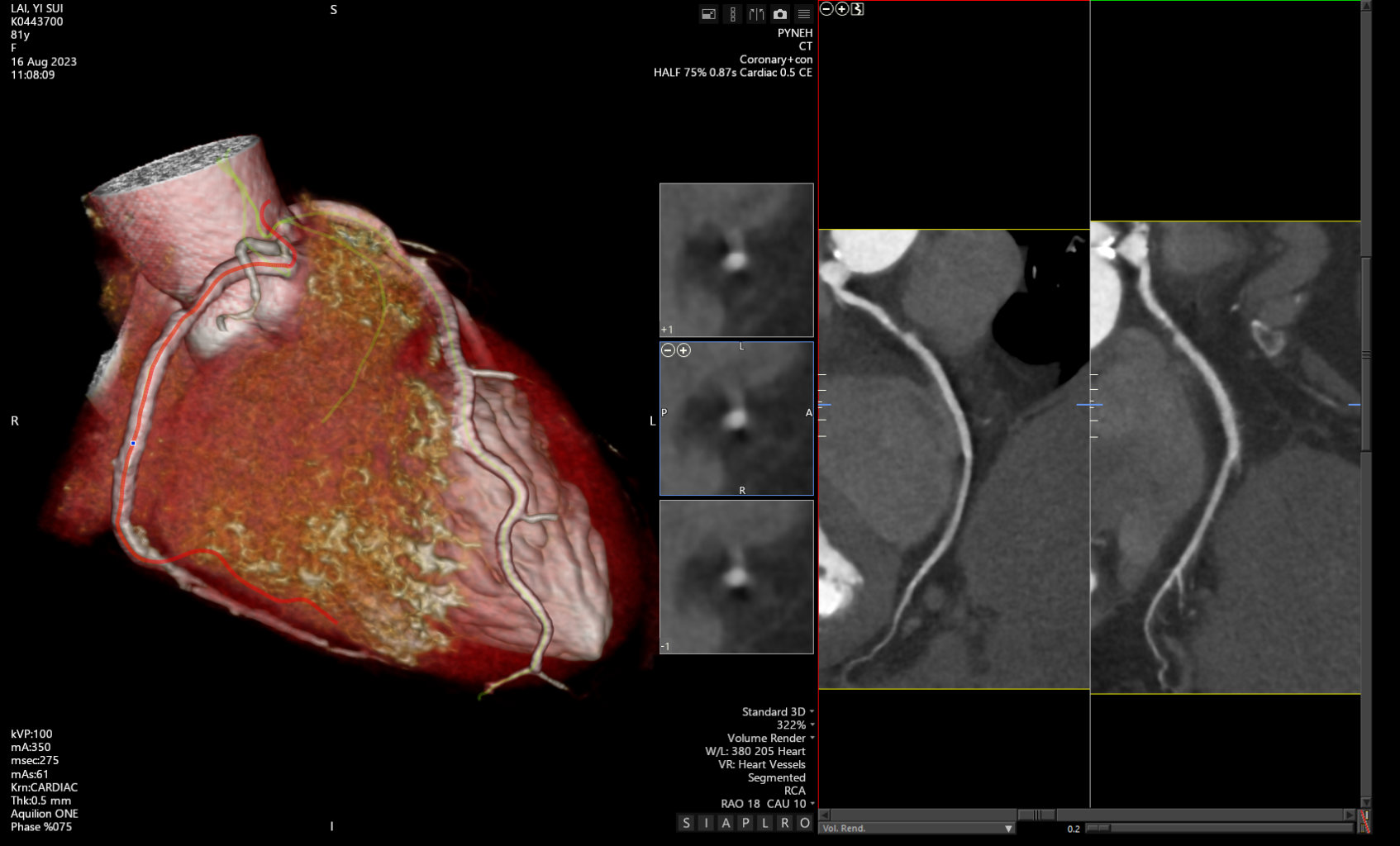
Baseline renal function showed an eGFR 50 mL/min/1.73m2. Hemoglobin A1c 6.8% and LDL-c 2.6 mmol/L.ECG showed normal sinus rhythm.CT coronary angiogram in 2023 showed moderate proximal RCA stenosis.
Relevant Catheterization Findings
Coronary angiogram on 14 January 2025 showed mid LAD 20% and proximal RCA 80% stenosis.
 Pre RCA LAO CRA.mp4
Pre RCA LAO CRA.mp4
 Pre RCA RAO CRA.mp4
Pre RCA RAO CRA.mp4
Interventional Management
Procedural Step
Right radial access was established. JR guiding catheter was used to engage RCA. RCA was wired with NS Runthrough and IVUS was used to assess the lesion. The proximal RCA lesion was pre-dilated with a 2.25 semi-compliant balloon and a 3.5 x 38 mm DES was deployed across the lesion covering to ostial RCA. The stent was post-dilated with 3.5 non-compliant balloon along its length. IVUS confirmed adequate expansion of the stent with good apposition. Angiogram showed distal PLV perforation due to guidewire trauma. PLV was re-wired with microcatheter support and continuous negative pressure was applied for flow occlusion whilst preparing for Vicryl embolization. Brief balloon tamponade was also performed in attempt to seal off the perforation site. Ultimately, two 3-0 Vicryl sutures were deployed to distal PLV with successful occlusion of the perforation site. Final angiogram confirmed no further contrast extravasation with sealing off the distal branches of PLV. Patient remained hemodynamically stable throughout the procedure with no symptoms of chest discomfort. Post-PCI echo confirmed no pericardial effusion and serial blood tests did not show any significant cardiac enzyme leak. She was subsequently discharged the following day and remained asymptomatic at follow-up.
 9 RCA RAO PLV perforation.mp4
9 RCA RAO PLV perforation.mp4
 17 Final RCA RAO.mp4
17 Final RCA RAO.mp4
 Vicryl embolization.mp4
Vicryl embolization.mp4
Case Summary
Management of coronary artery perforation requires identifying the rupture site. Often distal wire perforations are localised haematomas at the time of diagnosis and patients are generally stable. Therefore, there is time to decide on the best approach. According to the consensus document published by the Japanese Society for Cardiovascular Intervention and Therapeutics, clearly identifiable distal perforations can be managed by embolisation of coil, thrombus, fat and gel foam. We used a novel embolisation method using Vicryl sutures with good success. The experience of using this technique was first shared by Dr Lam Ho from HK and should be considered a possible option in selected cases.
