CASE20250807_001
Recurrent Inferior STEMI Due to Subacute Stent Thrombosis
By Hang Long Li, PAK HIN TAM, TSUN HO LAM, WANG HEI RICKY LEUNG, CHUN YIN JEFFREY LEE, LAP TIN LAM, KA CHUN TIMOTHY UN, KWONG YUE ERIC CHAN
Presenter
Hang Long Li
Authors
Hang Long Li1, PAK HIN TAM1, TSUN HO LAM1, WANG HEI RICKY LEUNG1, CHUN YIN JEFFREY LEE2, LAP TIN LAM2, KA CHUN TIMOTHY UN1, KWONG YUE ERIC CHAN2
Affiliation
Queen Mary Hospital, Hong Kong, China1, Grantham Hospital, Hong Kong, China2
View Study Report
CASE20250807_001
ACS/AMI - ACS/AMI
Recurrent Inferior STEMI Due to Subacute Stent Thrombosis
Hang Long Li1, PAK HIN TAM1, TSUN HO LAM1, WANG HEI RICKY LEUNG1, CHUN YIN JEFFREY LEE2, LAP TIN LAM2, KA CHUN TIMOTHY UN1, KWONG YUE ERIC CHAN2
Queen Mary Hospital, Hong Kong, China1, Grantham Hospital, Hong Kong, China2
Clinical Information
Relevant Clinical History and Physical Exam
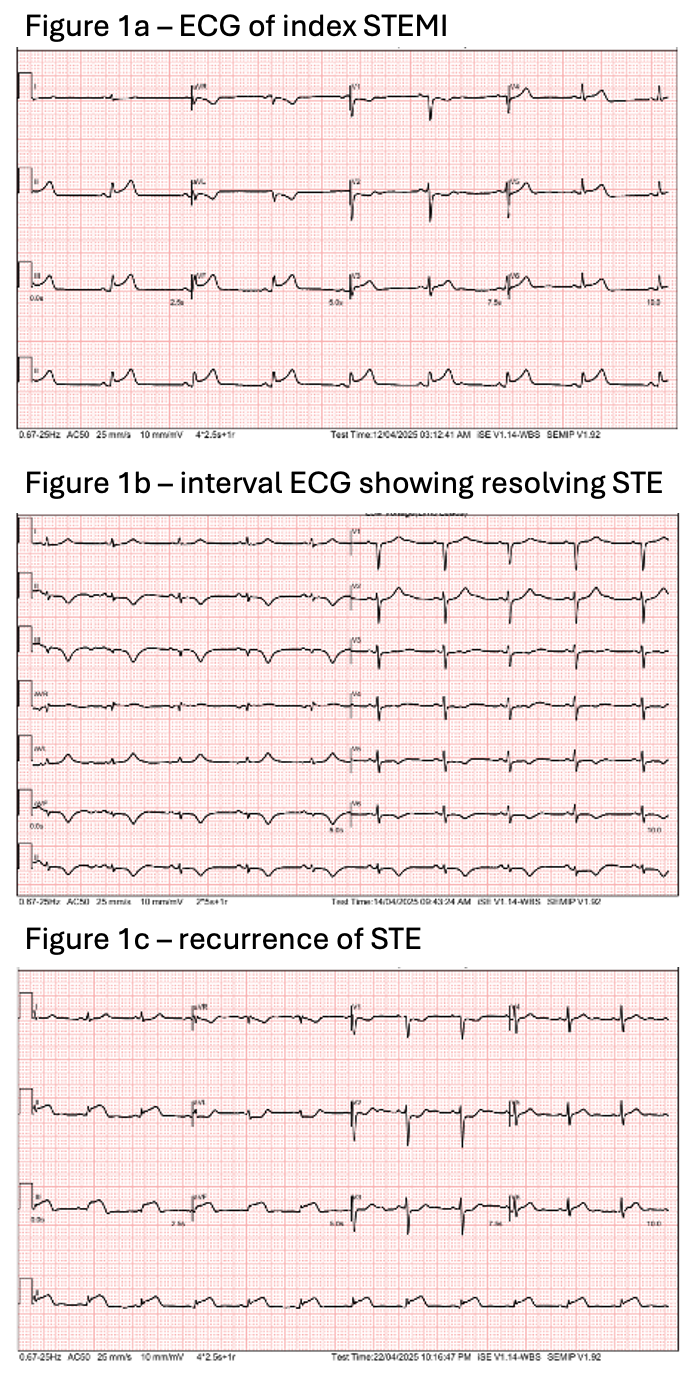
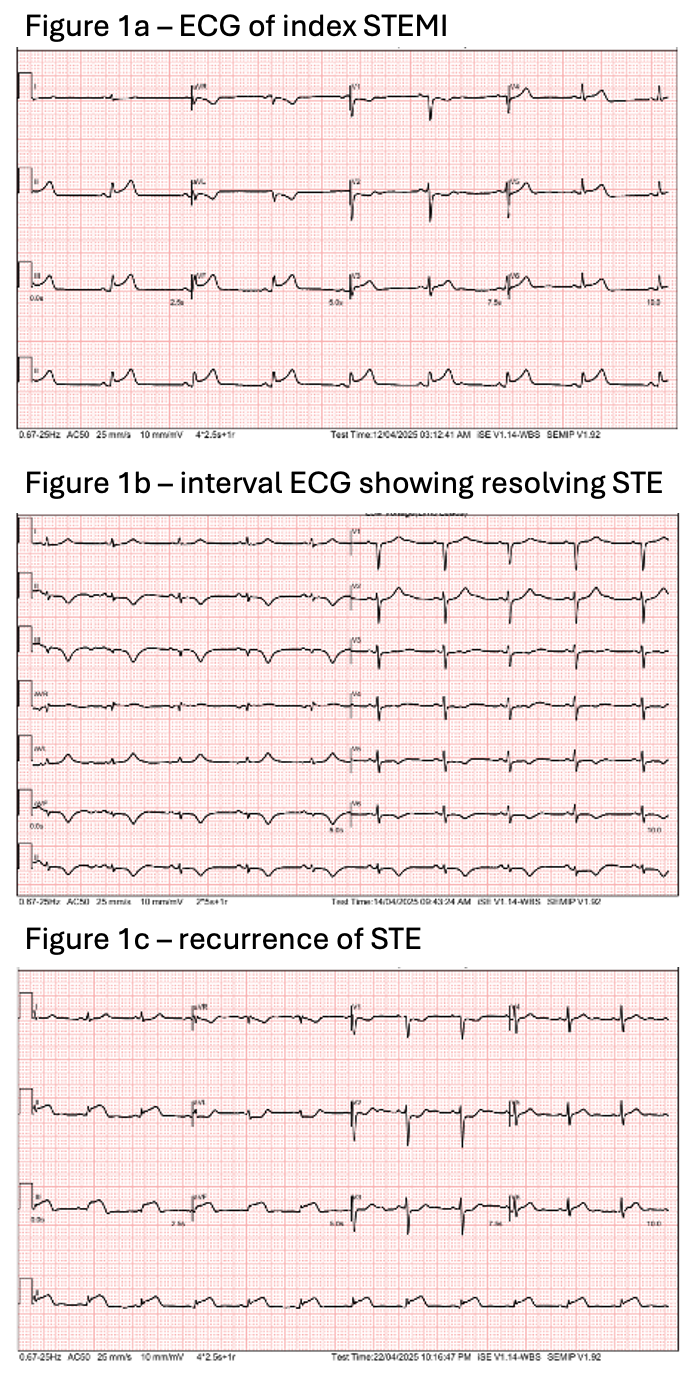
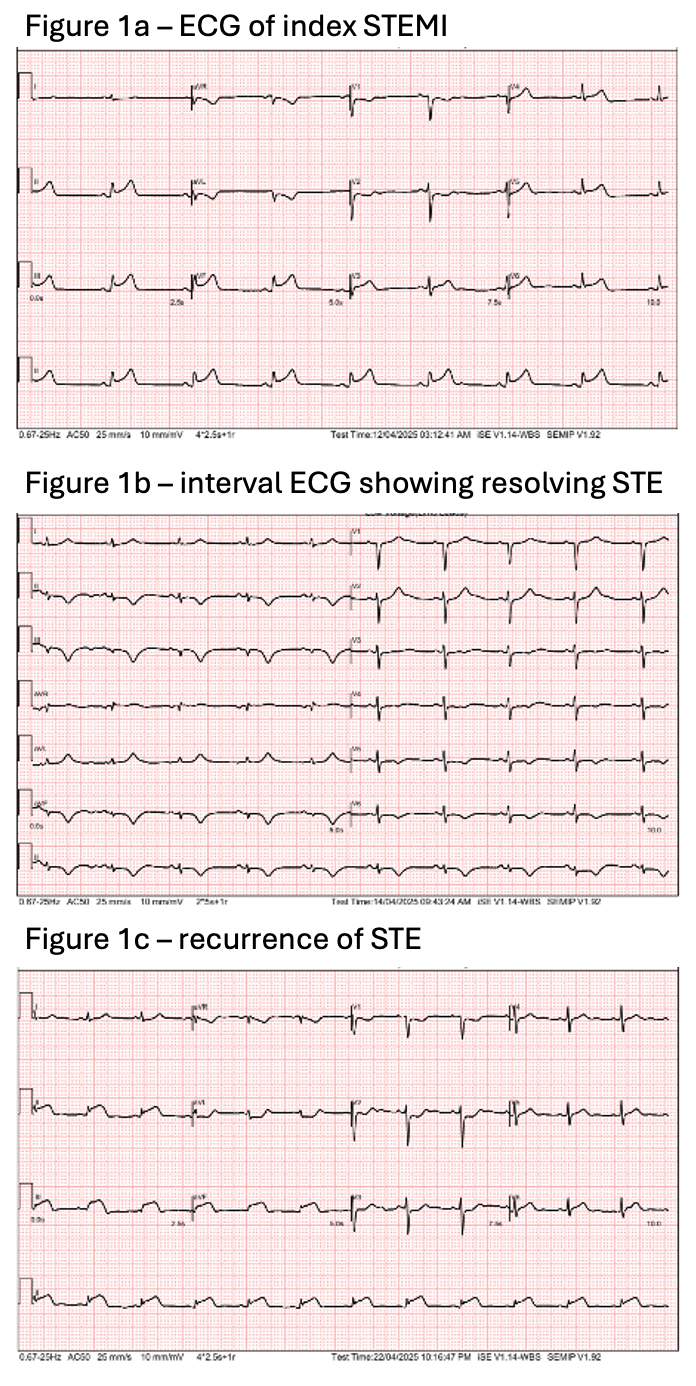
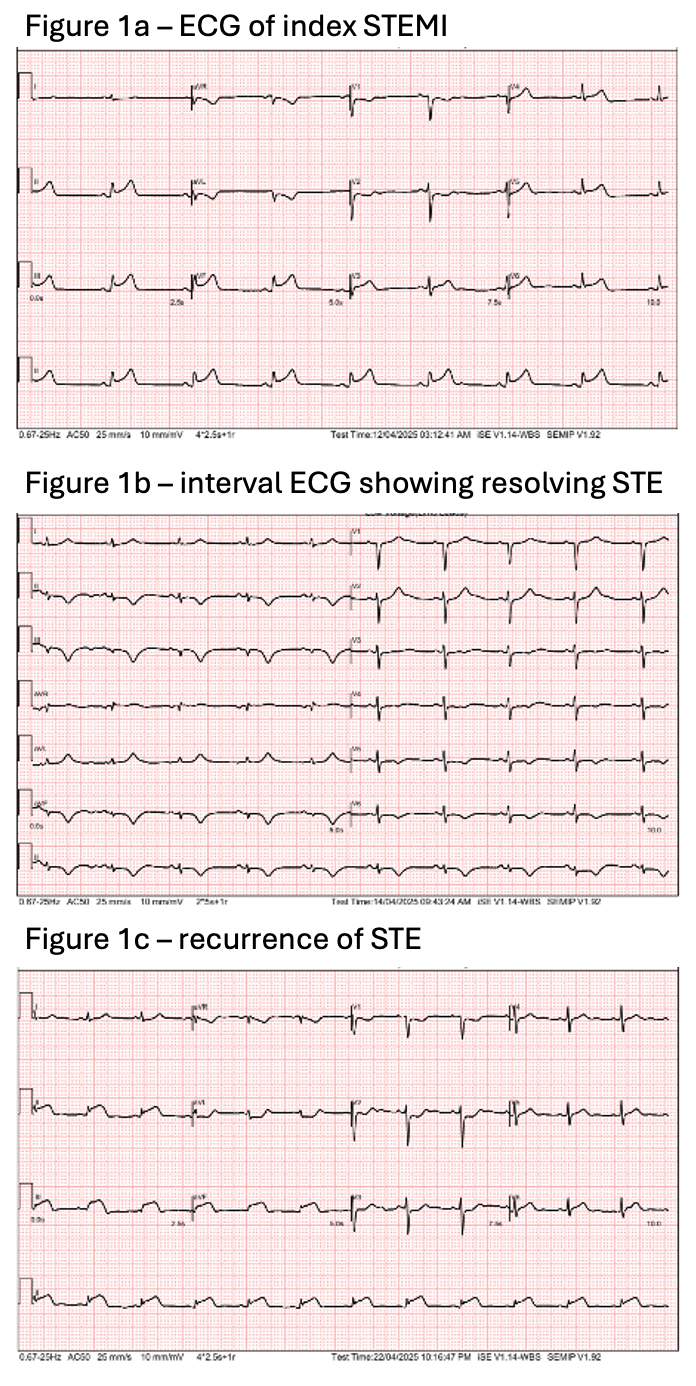
A 65-year-old female smoker with history of atrial fibrillation presented with inferior STEMI and underwent primary PCI to RCA. She was treated with triple therapy (apixaban, aspirin, clopidogrel) for 1 week, then continued on apixaban plus clopidogrel while awaiting staged PCI to left system. At discharge, ST elevation had resolved. Eleven days later, she re-presented with acute chest pain and was again diagnosed with inferior STEMI (Figure 1). She reported strict compliance with medications.
Relevant Test Results Prior to Catheterization
ECG of the patient showed recurrence of ST elevation over inferior leads (Figure 1). Echocardiogram revealed left ventricular ejection fraction (LVEF) of 50% with hypokinetic inferior wall.
Relevant Catheterization Findings
Cardiac catheterization revealed diffuse subacute stent thrombosis, with 70% stenosis over mid-RCA (Video 1). There was 70% stenosis over mid-LAD as well as proximal-mid-LCX. LM was normal.
 Video 1.mov
Video 1.mov
Interventional Management
Procedural Step
RCA was engaged with 5Fr JR4 via RRA and the posterior descending artery (PDA) was wired with Sion Blue. OCT was done, showing diffuse red and white thrombosis (Video 2), with no significant stent underexpansion/malopposition and edge dissection. Boluses of Eptifibatide was given followed by infusion. Plain-old balloon angioplasty (POBA) was performed using NC Trek 3.5mm, NC Euphora 3.5mm, and NC Trek 4.0mm. After POBA, angiogram revealed excellent results with TIMI 3 flow (Video 3). Final OCT revealed improved stent expansion with significant reduction in thrombus load (Video 4). The patient subsequently underwent staged PCI to the left system 1 month later. Genetic testing for clopidogrel resistance was prompted by (i) subacute stent thrombosis occurring 11 days after index intervention, (ii) development of symptoms shortly after stepping down from triple antithombotic therapy, (iii) good drug compliance, and (iv) no significant evidence of stent underexpansion/malopposition and edge dissection on OCT. There was homozygous mutation over CYP 2C19*2, and the patient was regarded as a poor metabolizer at risk of poor response to clopidogrel. After completion of triple antithrombotic therapy (apixaban, aspirin, and clopidogrel) for an extended period of 1 month, the patient was kept on apixaban with aspirin.
 Video 2.mov
Video 2.mov
 VIdeo 3.mov
VIdeo 3.mov
 Video 4.mov
Video 4.mov
Case Summary
The patient developed recurrent STEMI over RCA. Angiogram and OCT revealed stent thrombosis, and primary PCI was performed. Use of clopidogrel was avoided and the patient remained well on apixaban plus aspirin.This case illustrates the potential disastrous consequences of undiagnosed clopidogrel resistance and the importance of high clinical suspicion towards it. In high-risk populations and in patients with good drug compliance without obvious alternative cause for early stent thrombosis, a low threshold for genetic testing should be adopted. Further research is warranted to better define testing threshold.
