CASE20250809_001
A Step by Step Rotablation for Severe Calcified Left Main and Left Circumflex Ostial Lesion
By Woong Gil Choi
Presenter
Woong Gil Choi
Authors
Woong Gil Choi1
Affiliation
Chungbuk National University Hospital, Korea (Republic of)1
View Study Report
CASE20250809_001
Complex PCI - Calcified Lesion
A Step by Step Rotablation for Severe Calcified Left Main and Left Circumflex Ostial Lesion
Woong Gil Choi1
Chungbuk National University Hospital, Korea (Republic of)1
Clinical Information
Relevant Clinical History and Physical Exam
A 74-year-old male with a history of diabetes mellitus and hypertension was transferred from a local hospital. Two weeks earlier, the patient had undergone percutaneous coronary intervention (PCI) for a mid–left anterior descending (mLAD) artery lesion. During the same admission, an attempt was made to treat an ostial lesion of the left circumflex (LCX) artery; however, the procedure was unsuccessful, and the patient was referred to our hospital for further management.
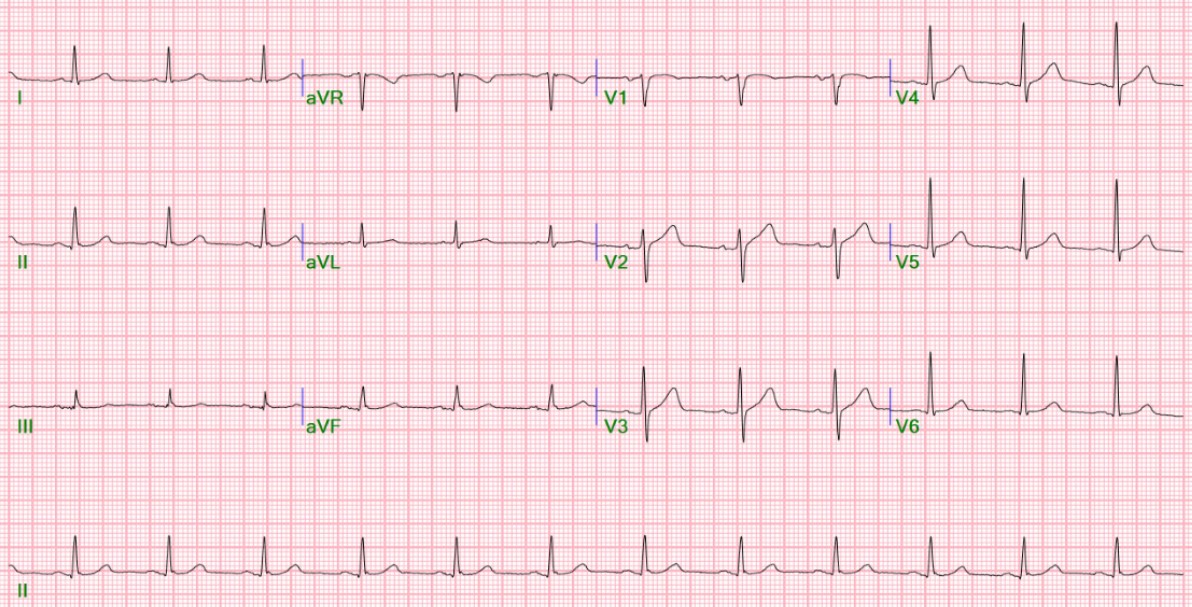
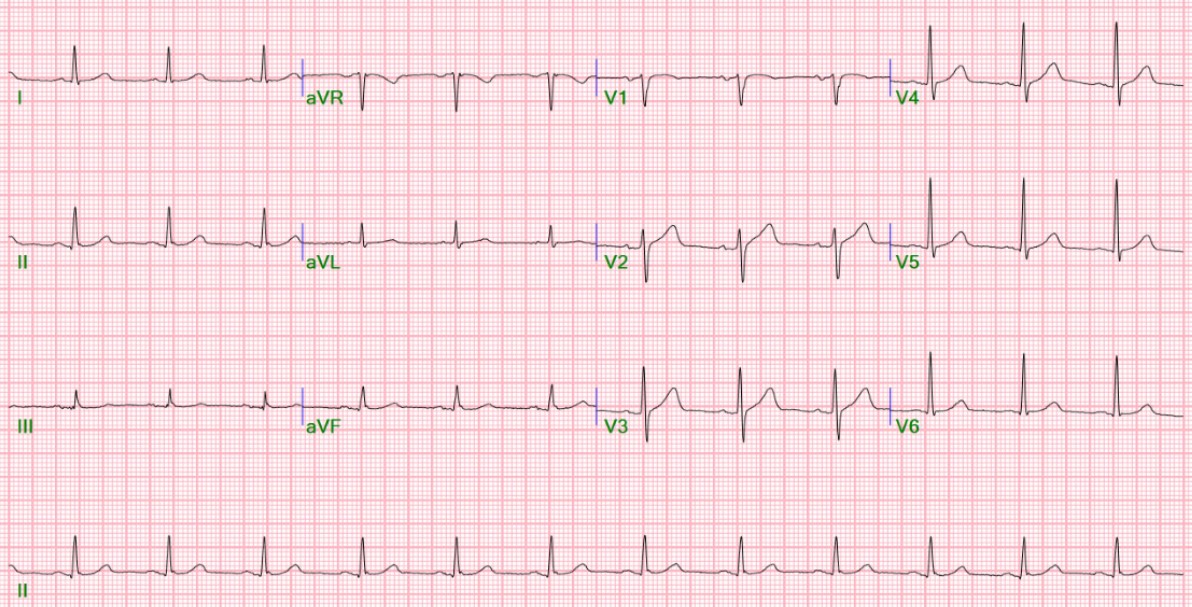
Relevant Test Results Prior to Catheterization
On admission, transthoracic echocardiography revealed no regional wall motion abnormalities.
Relevant Catheterization Findings
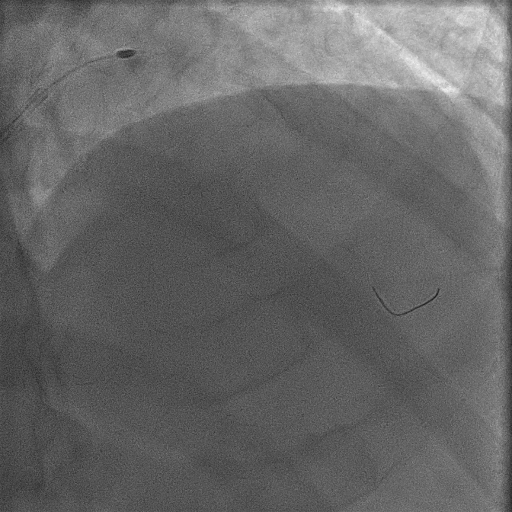
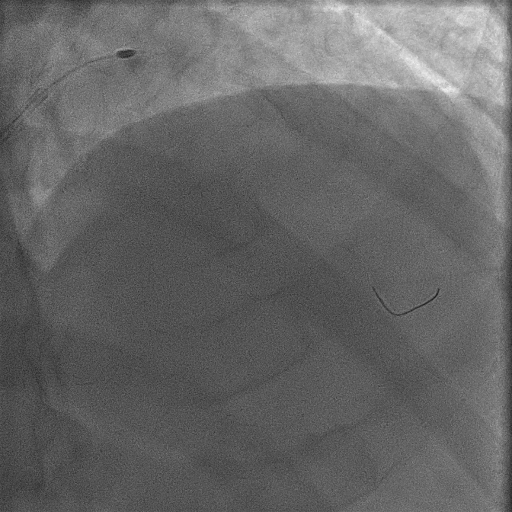
Coronary angiography demonstrated a sharp, heavily calcified protrusion in the distal left main artery, with contiguous calcification involving the LCX ostium and producing significant luminal stenosis. An intravascular ultrasound (IVUS) examination was attempted to better characterize the plaque morphology; however, the IVUS catheter could not be advanced across the left main lesion.
 LAO caudal.mp4
LAO caudal.mp4
 Calcification to the LCX_AP caudal.mp4
Calcification to the LCX_AP caudal.mp4
Interventional Management
Procedural Step
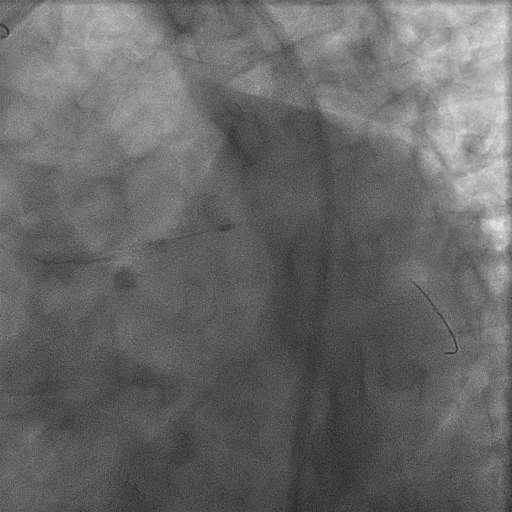
Subsequently, wiring of the LCX artery was attempted. Conventional wiring failed due to a protruding calcified lesion at the LCX ostium. Sequential wiring attempts were made using a Corsair microcatheter(CM, Asahi Intecc Co. Ltd, Aichi, Japan), a SuperCross 90° catheter(Vascular Solutions, Inc.,Minneapolis, MN), and a Crusade dual-lumen catheter (Kaneka, Japan), but all were unsuccessful. Given the difficulty in crossing, we decided to modify the protruding calcified plaque first by performing rotational atherectomy with a 1.75-mm burr. Following this, wiring was successfully achieved using a GAIA Next 1 guidewire(Asashi Intecc, Japan). Despite successful wiring, plain old balloon angioplasty (POBA) produced suboptimal results. Therefore, an additional rotational atherectomy with a 1.5-mm burr was performed. After successful lesion modification, IVUS of the LCX was obtained, and PCI was completed using a two-stent crush technique using Synergy XD 3.5 x 16 mm for Lt main – pLAD and Synergy XD 3.0 x 16 mm for Lt main - pLCX
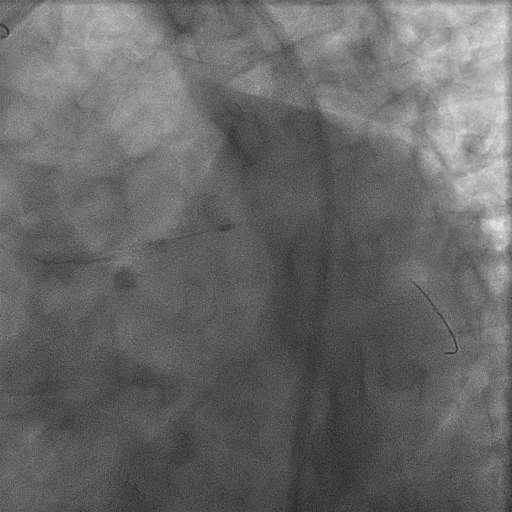
 Final LAO Caudal.mp4
Final LAO Caudal.mp4
Case Summary
A protruding calcified lesion of the left main coronary artery can pose significant challenges during PCI, particularly when located at a bifurcation. In such cases, lesion wiring is often difficult, and subsequent stent optimization may also be compromised. In these situations, initiating rotational atherectomy on the involved contralateral segment before performing sequential atherectomy on the primary target lesion can facilitate optimal plaque modification and improve the likelihood of procedural success in PCI.
