CASE20250812_003
“CHIP With Minimal Flavor”: Navigating Complexity With Ultra Low Contrast PCI and Impella Support
By I Gede Sumantra, Billal Patel, Rajinikanth Rajagopal
Presenter
I Gede Sumantra
Authors
I Gede Sumantra1, Billal Patel2, Rajinikanth Rajagopal2
Affiliation
Paramarta Cardiovascular Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2
View Study Report
CASE20250812_003
High-Risk Intervention - High-Risk Intervention (Diagetes, Heart Failure, Renal Failure, Shock, etc)
“CHIP With Minimal Flavor”: Navigating Complexity With Ultra Low Contrast PCI and Impella Support
I Gede Sumantra1, Billal Patel2, Rajinikanth Rajagopal2
Paramarta Cardiovascular Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2
Clinical Information
Relevant Clinical History and Physical Exam
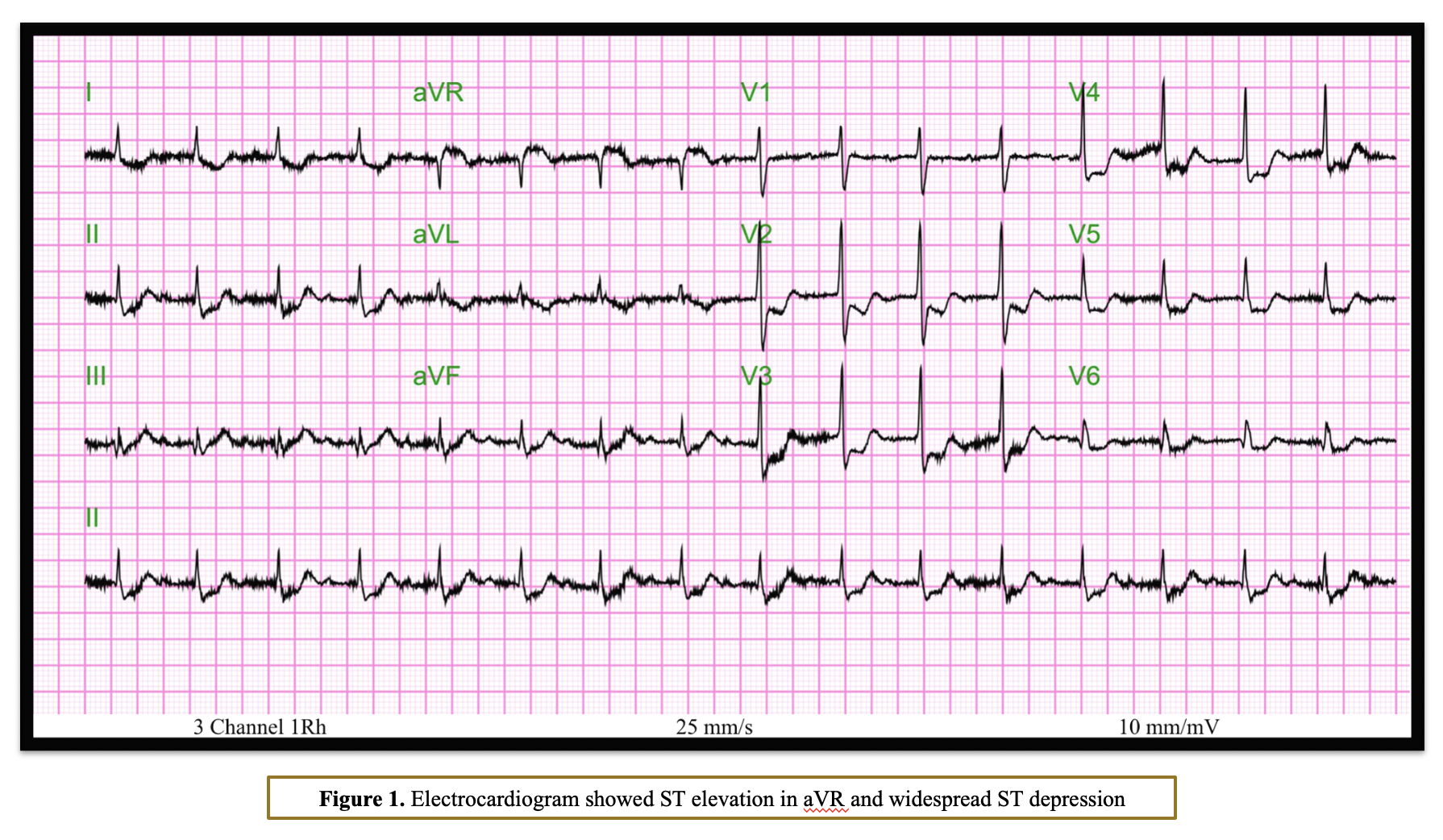
An 81-year-old male presented to the emergency department with NSTEMI and cardiogenic shock. His past medical history included hypertension, type II diabetes, peripheral vascular disease, and CKD stage IV (estimated glomerular filtration rate [eGFR] 17 mL/min/1.73 m²). An electrocardiogram (ECG) showed ST elevation in aVR and widespread ST depression.
Relevant Test Results Prior to Catheterization
Echocardiography indicated severe left ventricular systolic dysfunction (LVSD).
Relevant Catheterization Findings
Coronary angiography revealed severe calcified stenosis at the ostial left main (LM), severe disease in the proximal and mid-left anterior descending artery (LAD), and severe ostial left circumflex (LCx) artery disease. After discussion with the heart team, it was decided to proceed with Impella-supported ultra-low contrast PCI due to the high surgical risk associated with the patient’s impaired LV function and personal preference.


Interventional Management
Procedural Step
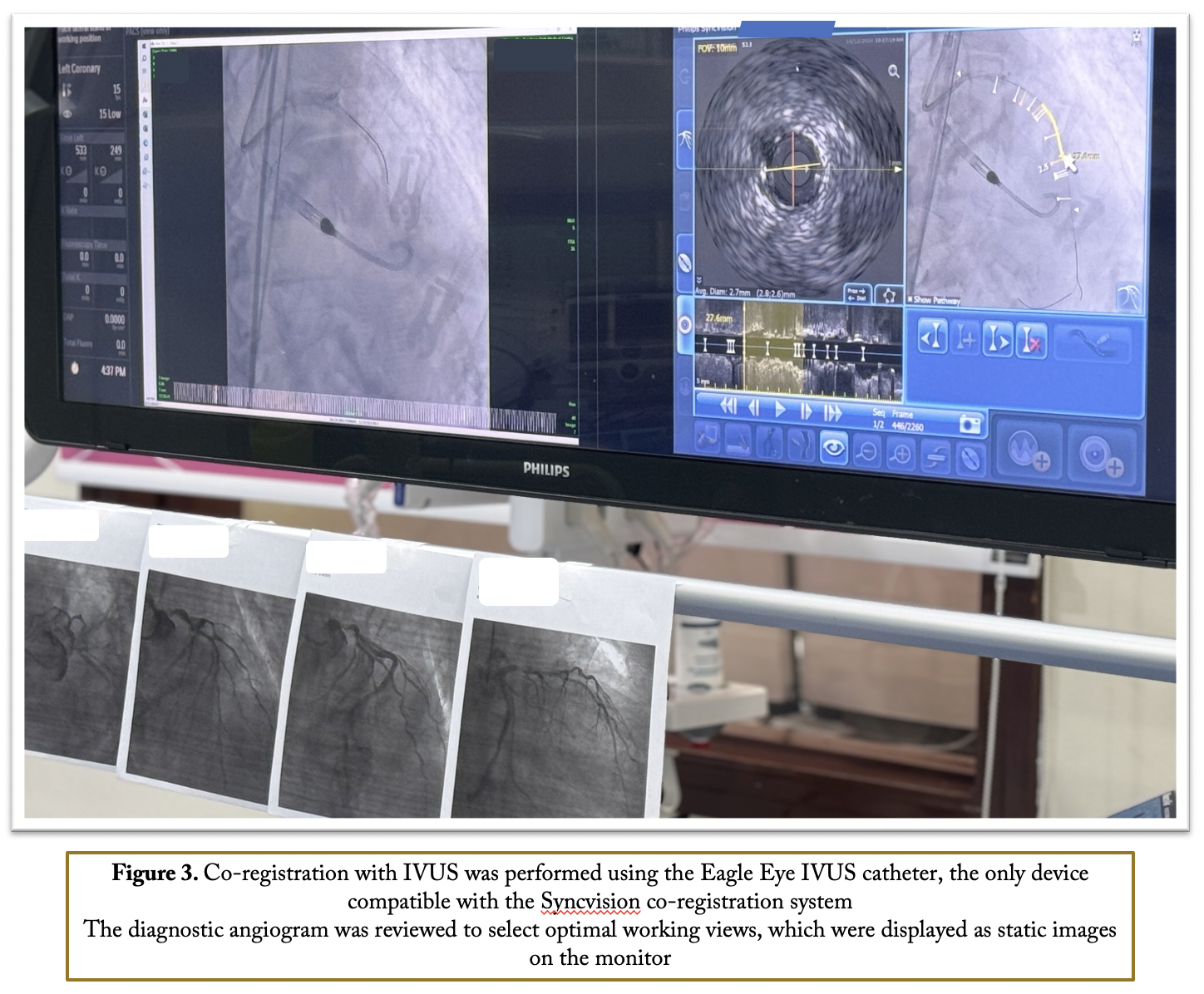
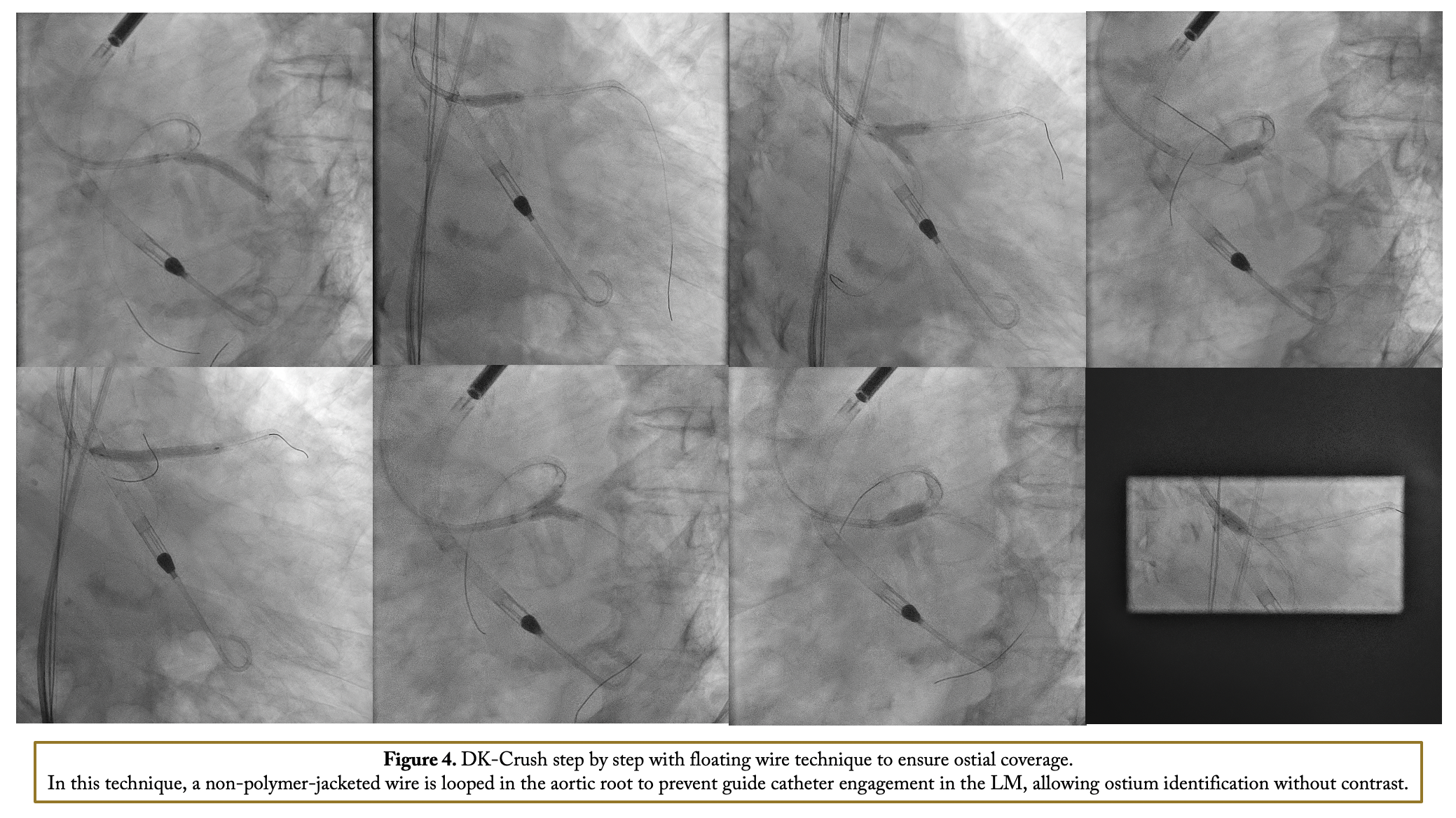
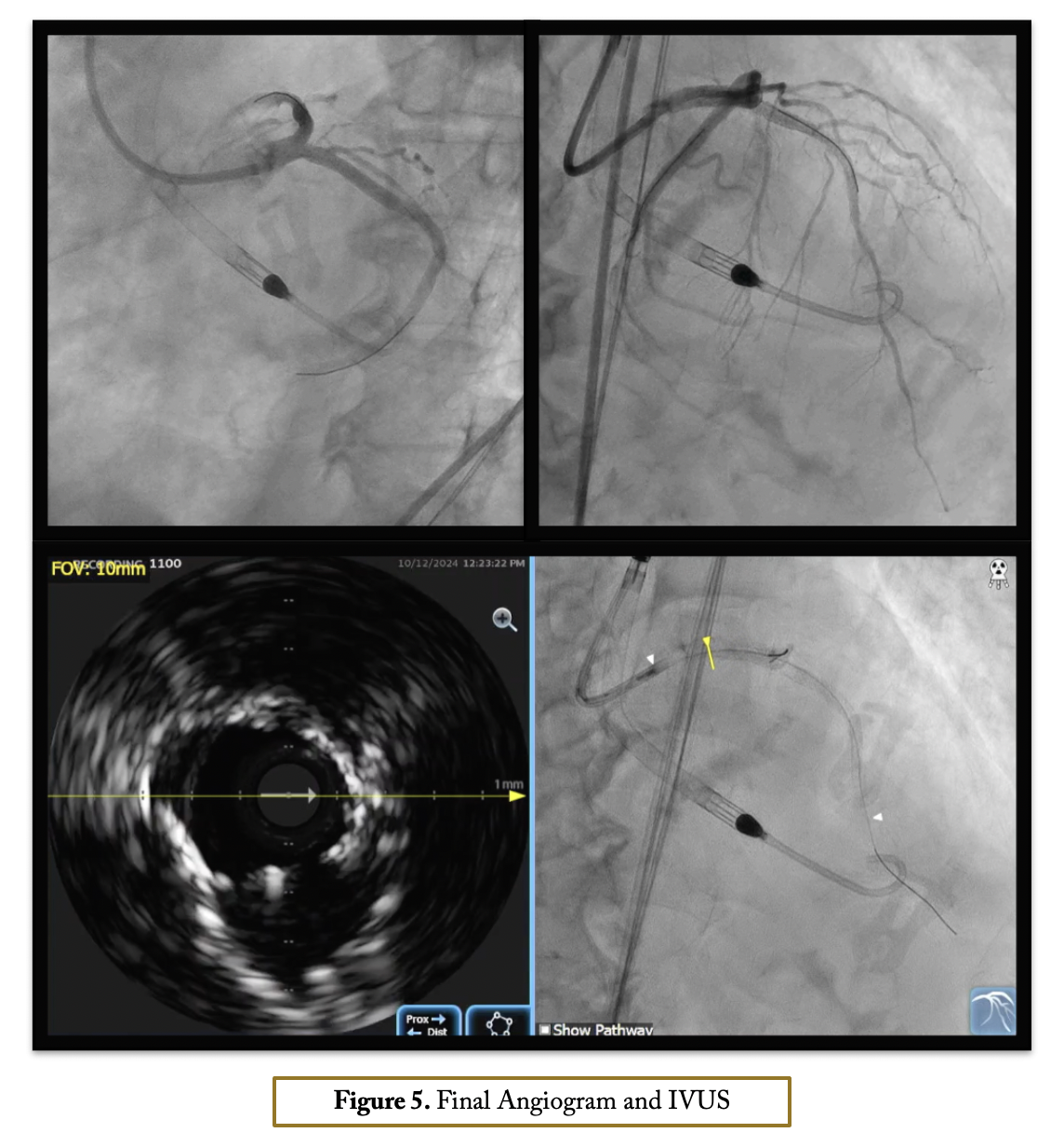
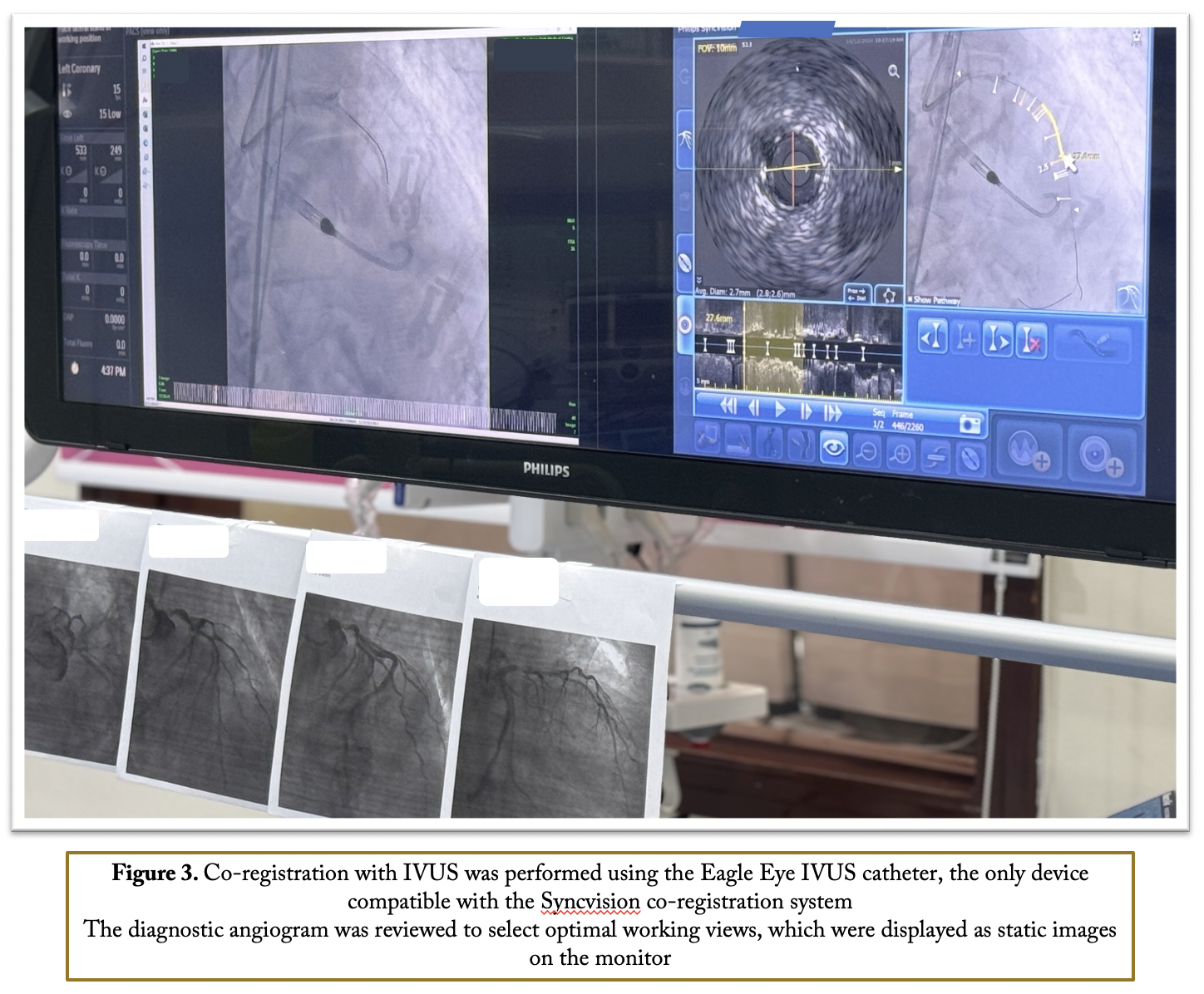
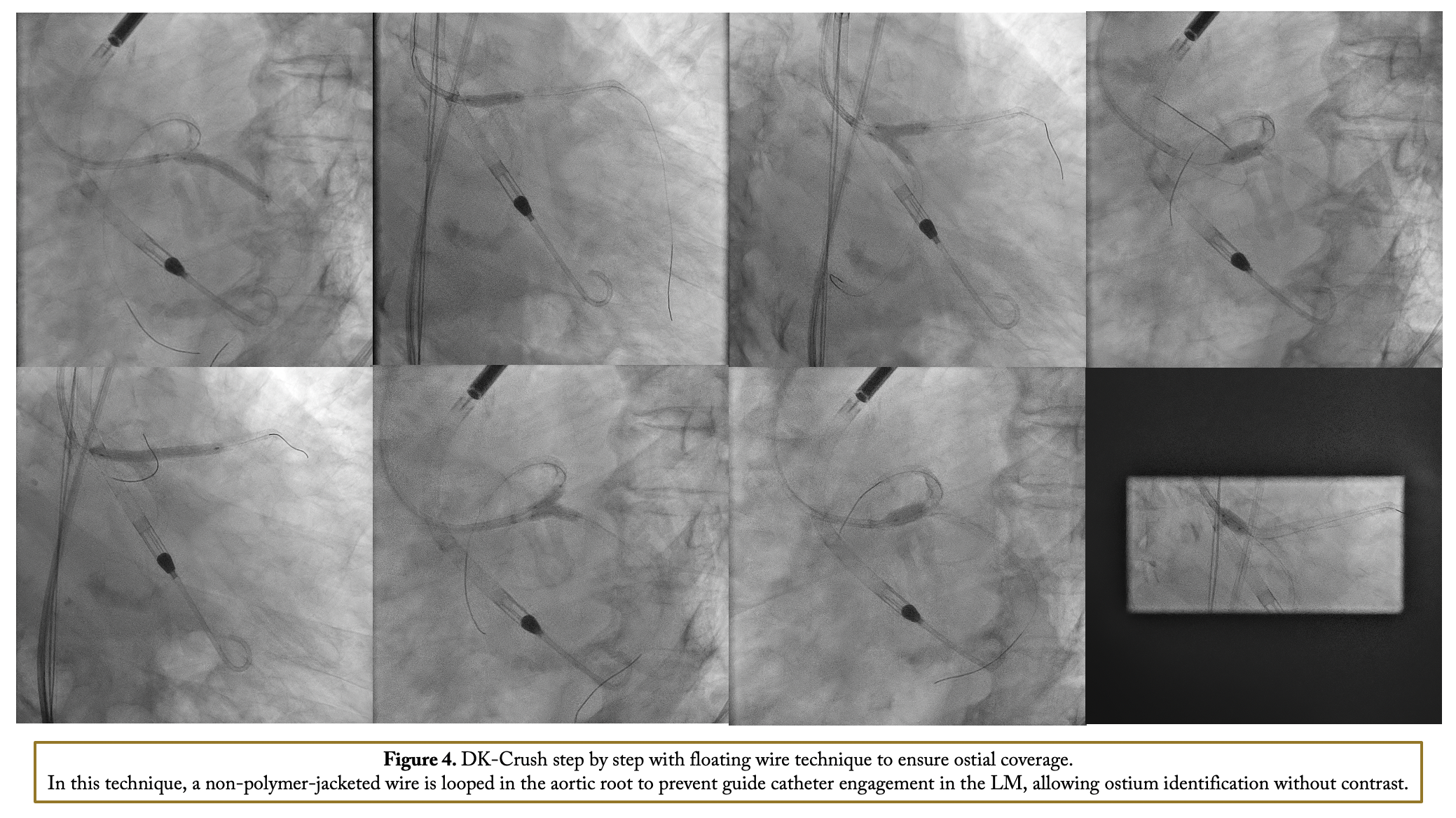
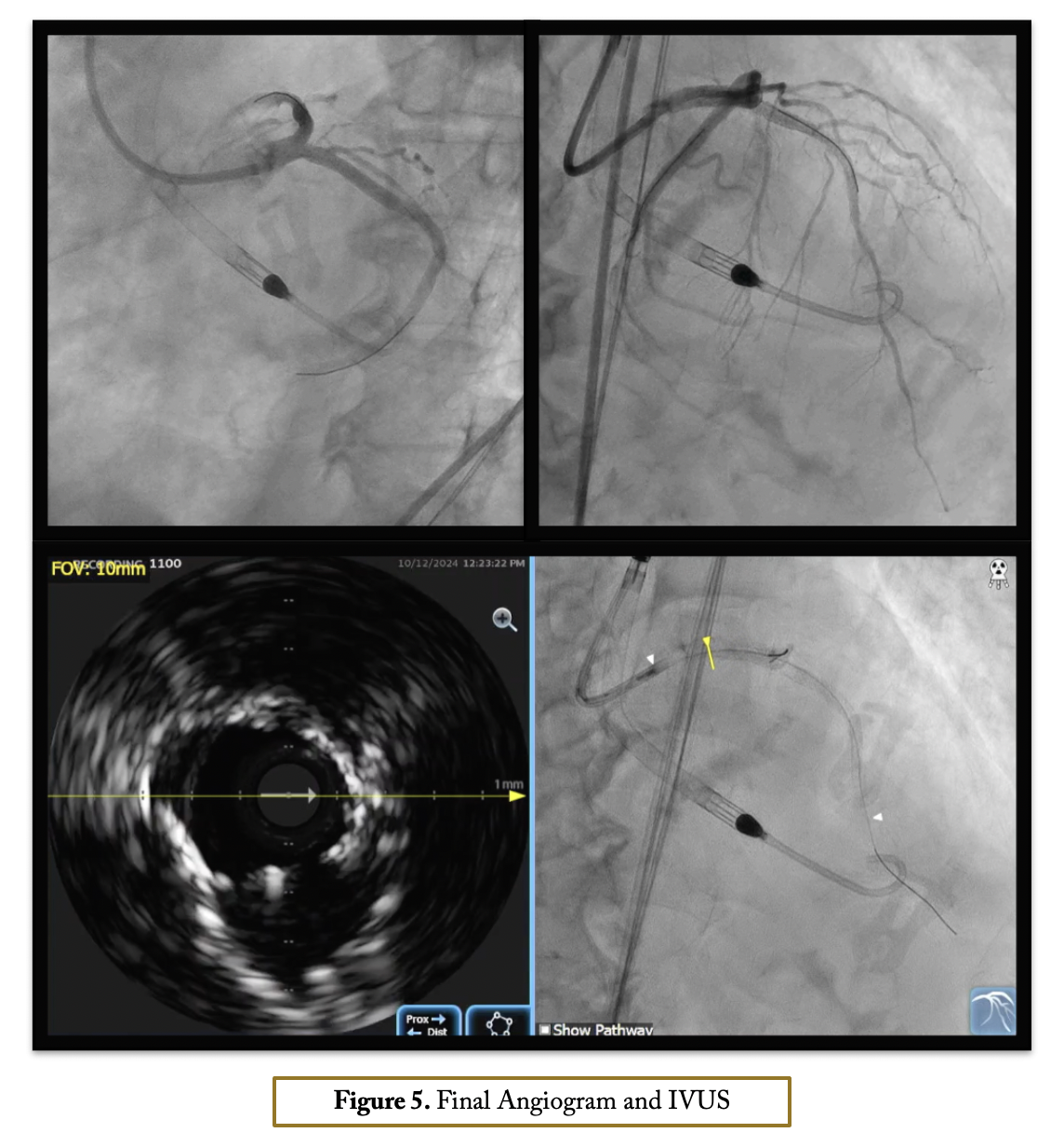
After confirming iliofemoral anatomy suitability for Impella via intravascular ultrasound (IVUS), right femoral access was obtained with a 14-Fr introducer and two suture-mediated closure devices. Diagnostic angiogram views were set as static monitor images. A 7-Fr sheath was inserted through the Impella introducer, and an EBU 3.5 7-Fr guide catheter engaged the left main coronary without contrast, aided by pressure damping, calcification identification, ECG changes, and wire probing. Co-registration with IVUS was performed using the Eagle Eye IVUS catheter, the only device compatible with the Syncvision co-registration system. IVUS imaging of the left main-LAD revealed fibrocalcific plaque with up to 360-degree calcification in the LM-LAD and LCx. Stent landing zones and vessel sizes were identified, and IVUS imaging of the LCx confirmed severe ostial disease. Rotational atherectomy was done with a 1.5 mm burr in both LAD and LCx. Intravascular lithotripsy (IVL) with a 4.0 mm balloon was applied in the ostial LCx and LM with 120 pulses. The LM bifurcation was treated with a DK crush technique with a non-polymer-jacketed wire is looped in the aortic root to prevent guide catheter engagement in the LM, allowing ostium identification without contrast Final IVUS and angiogram showed good outcomes with stable hemodynamics via Impella support. Hemostasis was achieved with Proglide sutures after device removal.
Case Summary
Ultra-low contrast PCI with Impella support offers a feasible and effective option for complex, high-risk patients with severe renal impairment and hemodynamic instability. This case demonstrates that with careful imaging, lesion preparation, and hemodynamic support, ultra-low contrast PCI can be successfully performed in patients with calcified left main disease, reducing the risk of contrast-induced nephropathy and maintaining stable hemodynamic throughout the procedure.
