CASE20250818_001
Tackling Ostial Ambiguity in Left Main Bifurcation Disease: Strategic Retrograde Revascularization From Provisional to Two-Stent Approach
By Melly Susanti, Seung-Woon Rha
Presenter
Melly Susanti
Authors
Melly Susanti1, Seung-Woon Rha2
Affiliation
Ministry of Health Surabaya Hospital, Indonesia1, Korea University Guro Hospital, Korea (Republic of)2
View Study Report
CASE20250818_001
Complex PCI - CTO
Tackling Ostial Ambiguity in Left Main Bifurcation Disease: Strategic Retrograde Revascularization From Provisional to Two-Stent Approach
Melly Susanti1, Seung-Woon Rha2
Ministry of Health Surabaya Hospital, Indonesia1, Korea University Guro Hospital, Korea (Republic of)2
Clinical Information
Relevant Clinical History and Physical Exam
A 50-year-old male with a history of percutaneous coronary intervention (PCI) to the left circumflex (LCX) artery was transferred for evaluation of recurrent angina over the past three months. He had no history of hypertension, diabetes, or other significant comorbidities. He was a never-smoker, consumed alcohol occasionally, and had no relevant family history of cardiovascular disease.
Relevant Test Results Prior to Catheterization
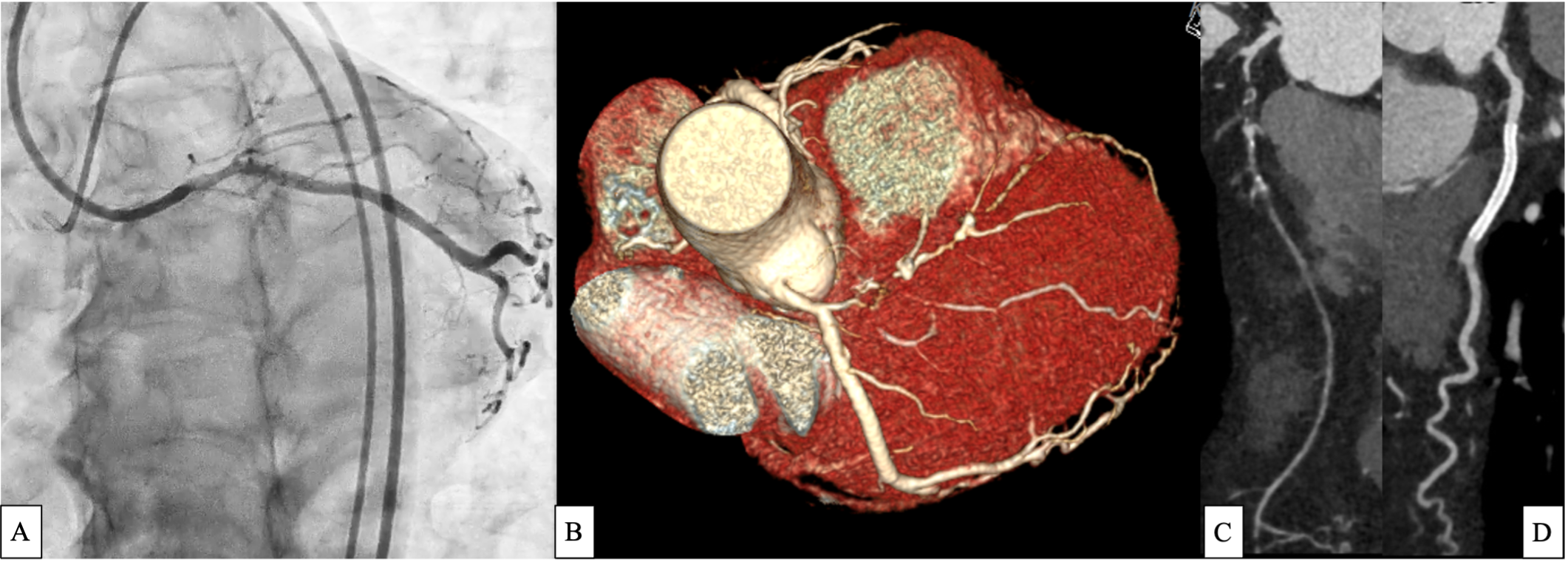
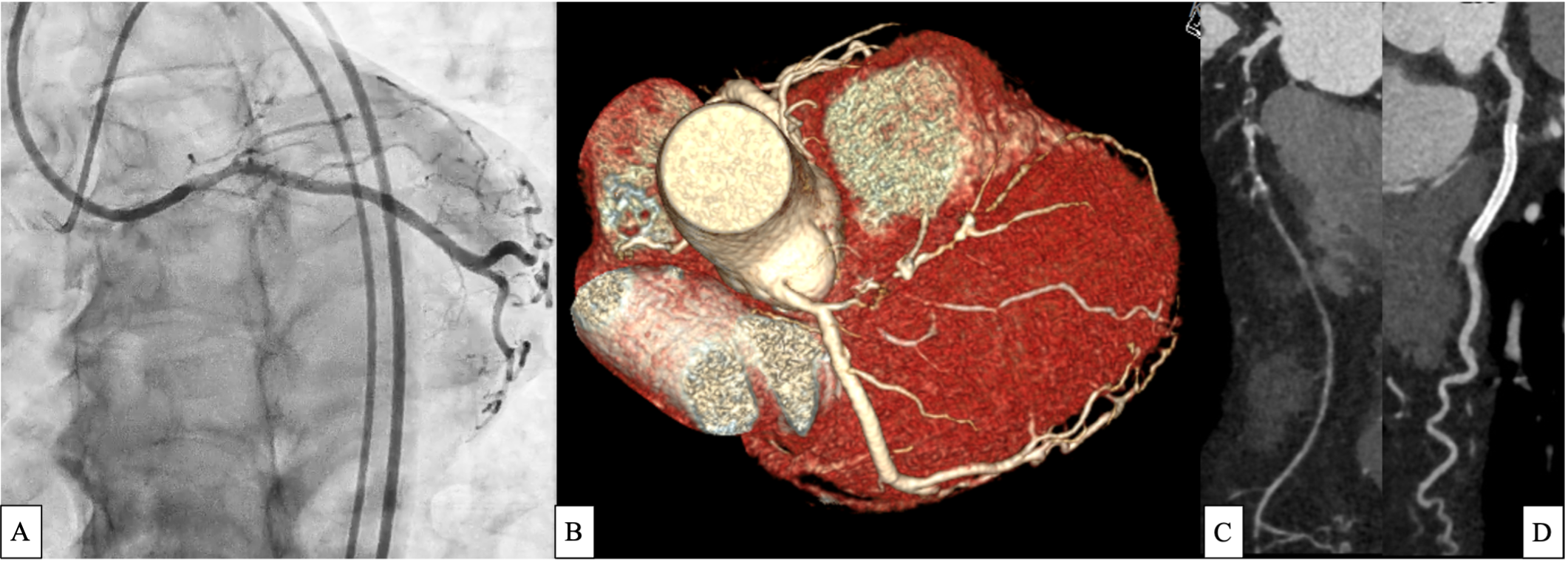
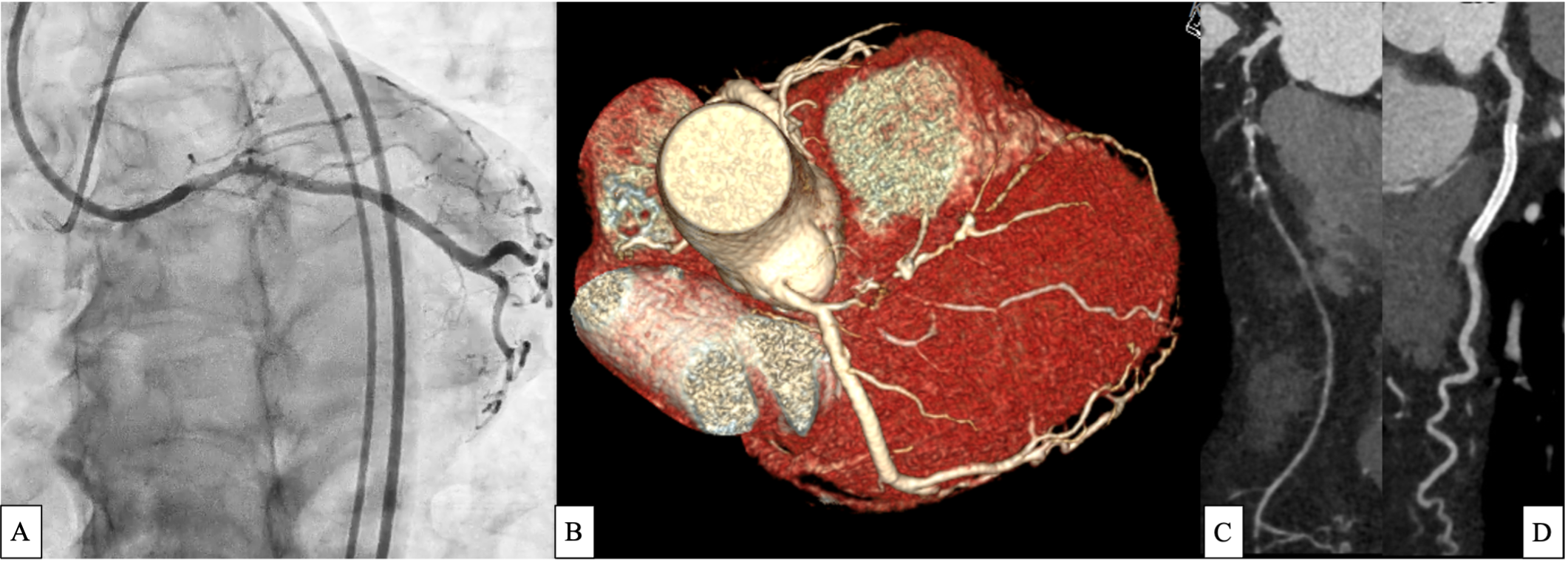
Coronary CT angiography (CCTA) revealed a right-dominant system with a noncalcified plaque causing approximately 50% stenosis in the left main (LM). The LAD proximal (including os) had a CTO with mixed plaque, measuring approximately 1.5 cm in length, while the mid LAD showed a severe (90%) mixed plaque stenosis, suggesting tandem high-grade lesions.
Relevant Catheterization Findings
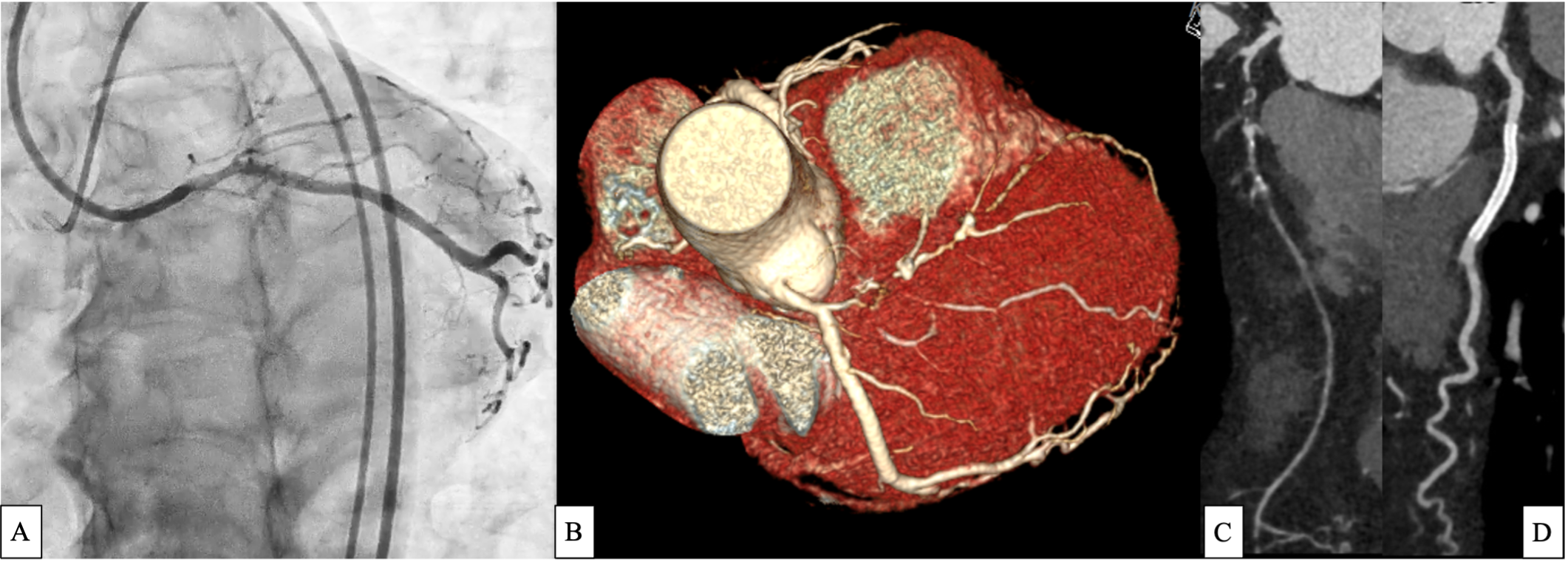
Invasive coronary angiography demonstrated a stumpless ostial LAD CTO lesion with well-developed septal collaterals from the RCA (Rentrop grade 3). Although retrograde tracking was technically challenging due to acute angulation at the septal–LAD connection, the LAD itself followed a relatively straight course, and the occlusion length was estimated to exceed 20 mm
 1. Dual contrast inj.mp4
1. Dual contrast inj.mp4
 2. CAG LAD.mp4
2. CAG LAD.mp4
 3. CAG RCA.mp4
3. CAG RCA.mp4
Interventional Management
Procedural Step
A brief anterograde approach was attempted. A wire was advanced into a high take-off obtuse marginal branch, and a dual-lumen microcatheter was positioned in the distal LM to redirect toward the occluded LAD. Multiple attempts with a dedicated penetration wire failed due to ambiguous proximal cap and possible injury, so the anterograde strategy was abandoned.The procedure was converted to retrograde. The RCA was engaged and a wire with microcatheter support advanced into distal septal collaterals. A softer wire failed to track the distal septal due to angulation, so a proximal septal collateral was used, allowing successful passage into the proximal LAD. After confirmation, an externalization wire was advanced to establish a stable rail.IVUS confirmed true lumen entry, LAD ostium identification, and heavy plaque burden. Sequential balloon dilatation was followed by overlapping stent implantation from mid LAD to the ostium. However, the wire had tracked into a septal branch, and stenting jailed the true LAD. The LAD was rewired through stent struts and reconstructed with an additional stent using a culotte technique.Subsequent angiography showed significant ostial LCX jailing. The LCX was rewired, predilated, and stented under balloon protection, followed by final kissing balloon inflation. Final angiography and IVUS confirmed restored bifurcation flow and optimal stent expansion and apposition.
 13. CAG septal caravel.mp4
13. CAG septal caravel.mp4
 36. Final after FKB spider.mp4
36. Final after FKB spider.mp4
 Faster IVUS POST.mov
Faster IVUS POST.mov
Case Summary
This case underscores that success in complex LAD CTO with LM bifurcation involvement relies on abandoning ineffective anterograde attempts early, adopting a retrograde strategy, and leveraging intravascular imaging for precise guidance. Wire misdirection and septal stent deployment can be salvaged through rewiring and advanced bifurcation techniques, emphasizing the importance of flexibility, imaging, and technical mastery. Operators must anticipate complications, maintain multiple bailout strategies, and adapt in real time to achieve durable outcomes in high-risk CTO PCI.
