CASE20250818_004
Stent or Stand Down?
By Susila Surya Darma
Presenter
Susila Surya Darma
Authors
Susila Surya Darma1
Affiliation
I.G.N.G. Ngoerah Hospital Bali, Indonesia1
View Study Report
CASE20250818_004
ACS/AMI - ACS/AMI
Stent or Stand Down?
Susila Surya Darma1
I.G.N.G. Ngoerah Hospital Bali, Indonesia1
Clinical Information
Relevant Clinical History and Physical Exam
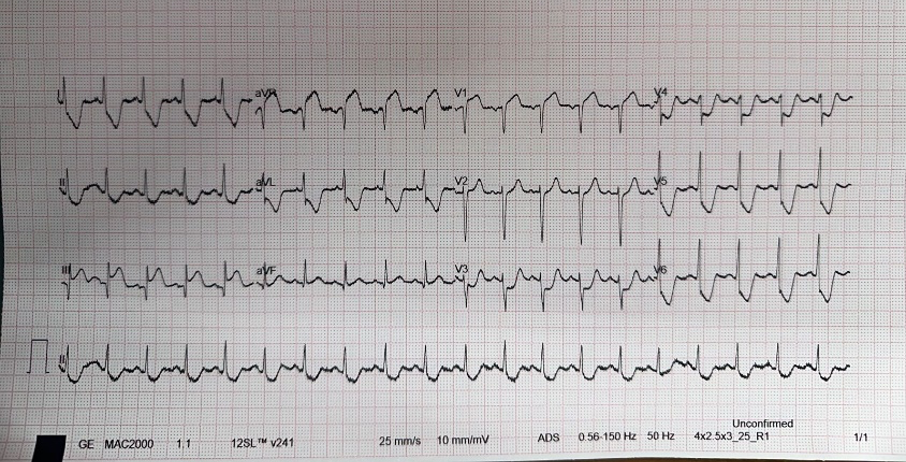
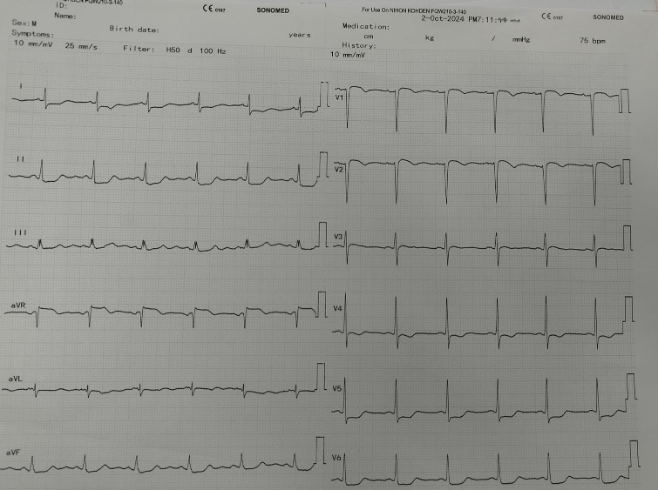
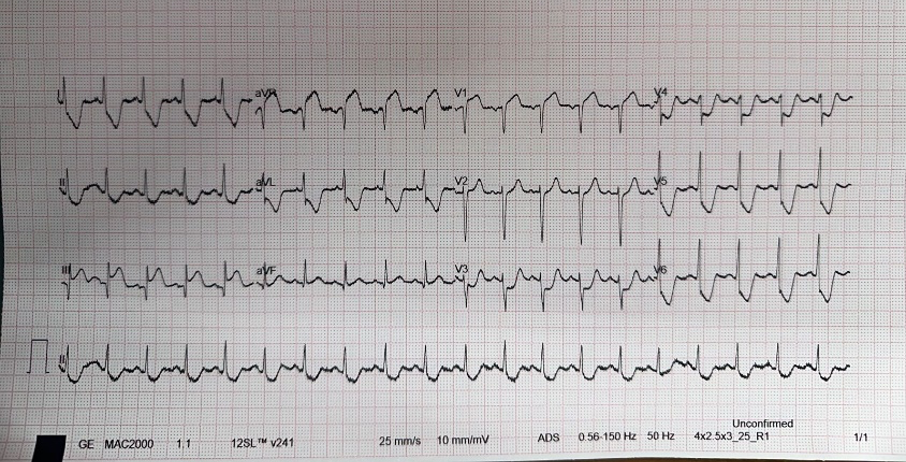
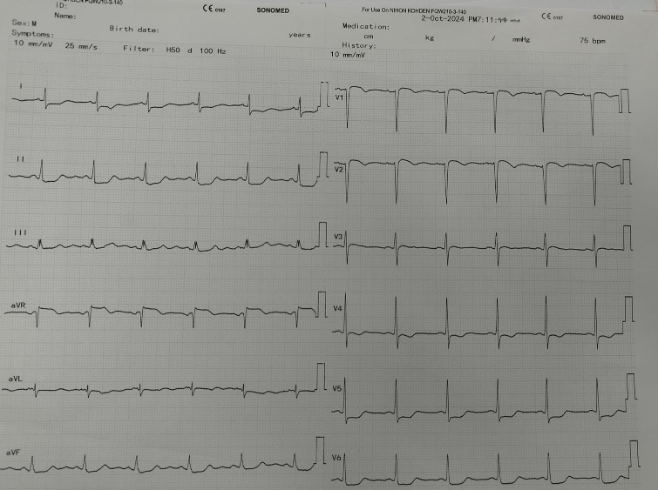
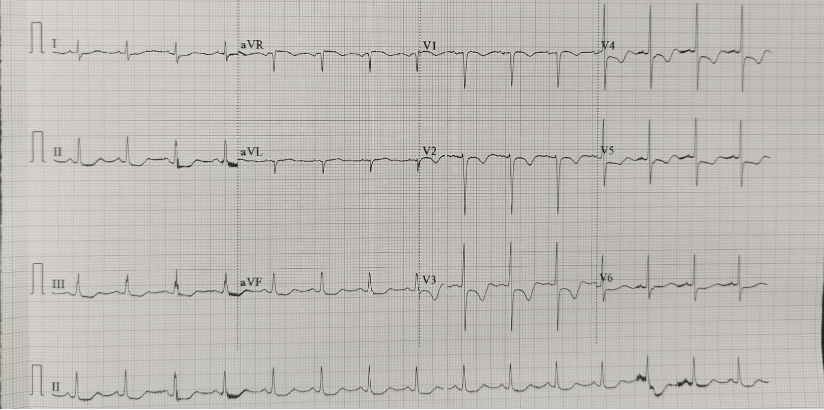
Case 1: A 49 yo, female with a history of hypertension and hyperthyroidism (on propranolol and thiamazole), presented with chest pain since 7-hours prior to admission. ECG: ST elevation at AVR.
Relevant Test Results Prior to Catheterization
Case 1: Vital signs: BP 120/80 mmHg, HR 100 bpm, RR 20/min, and SpO₂ 98% on room air. Labs: Blood glucose: 140 mg/dL; Serum creatinine: 0.64 mg/dL; hs-Troponin I: 67.6 µg/mL. Echo: EF: 58% ; TAPSE: 2.0 cm.
Relevant Catheterization Findings
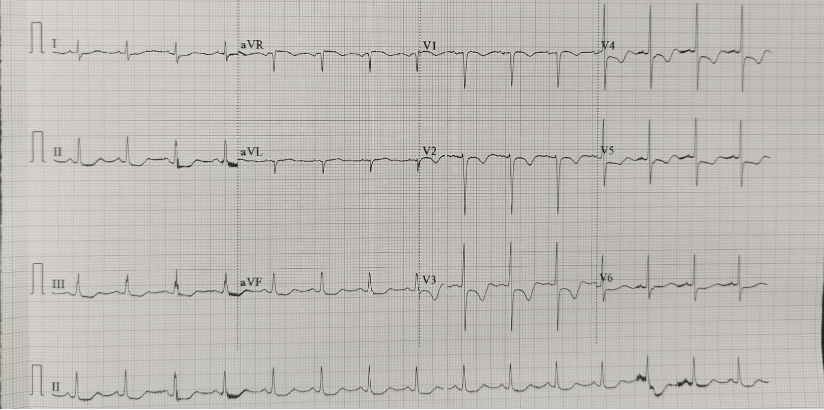
In both cases, coronary angiography revealed a critical lesion extending from the ostial LM artery to the proximal LAD artery. The LCx and RCA were angiographically normal.
 Cranial case 2.mp4
Cranial case 2.mp4
 Spider Case 2.mp4
Spider Case 2.mp4
 Spider Case 1.mp4
Spider Case 1.mp4
Interventional Management
Procedural Step
Case 1: a case of a patient with chest pain and stable hemodynamics, with angiographic findings suggestive of critical stenosis from ostial LM to pLAD. IVUS of the LAD revealed a MLA of pLAD: 9.29 mm², osteal LAD: 5.06 mm², and LM: 5.43 mm² without clear evidence of fixed stenosis. Intracoronary nitrate administration led to significant improvement in symptoms and ECG changes. IVUS showed marked improvement: MLA of osteal LAD: 8.67 mm² and LM: 8.34 mm². No intervention was performed. The patient remained symptom-free and hemodynamically stable during follow-up. At one-month post-discharge, the patient was asymptomatic on calcium channel blockers and long-acting nitrates.
 IVUS pre nitrat Case 1.mp4
IVUS pre nitrat Case 1.mp4
 IVUS post nitrat Case 1.mp4
IVUS post nitrat Case 1.mp4
 IVUS case 2 post DES.mp4
IVUS case 2 post DES.mp4
Case Summary
LM coronary artery spasm can occur spontaneously due to endothelial dysfunction or be induced iatrogenically. It typically responds well to vasodilator therapy. The first case was successfully managed with intracoronary vasodilators (nitrates), without the need for stenting. The second case showed persistent spasm and symptoms despite intracoronary vasodilators. Therefore, PCI with DES implantation was performed. PCI can be a safe and effective treatment option in selected patients with refractory left main spasm. Careful assessment is essential to determine whether conservative or interventional management is appropriate for LM coronary artery spasm.
