CASE20250822_004
Collaborative Cardiovascular Care: A Case of Integrating Vascular and Cardiology Strategies for High Risk Revascularisation
By Christina Mew, Darren Wong, Ping Wa Yam
Presenter
Christina Mew
Authors
Christina Mew1, Darren Wong1, Ping Wa Yam1
Affiliation
Tuen Mun Hospital, Hong Kong, China1
View Study Report
CASE20250822_004
Complex PCI - Multi-Vessel Disease
Collaborative Cardiovascular Care: A Case of Integrating Vascular and Cardiology Strategies for High Risk Revascularisation
Christina Mew1, Darren Wong1, Ping Wa Yam1
Tuen Mun Hospital, Hong Kong, China1
Clinical Information
Relevant Clinical History and Physical Exam
A 71-year-old previously active gentleman presented with a NSTEMI. Comorbidities include non insulin dependent diabetes mellitus and hypertension. He had no clinical signs of decompensated heart failure.
Relevant Test Results Prior to Catheterization
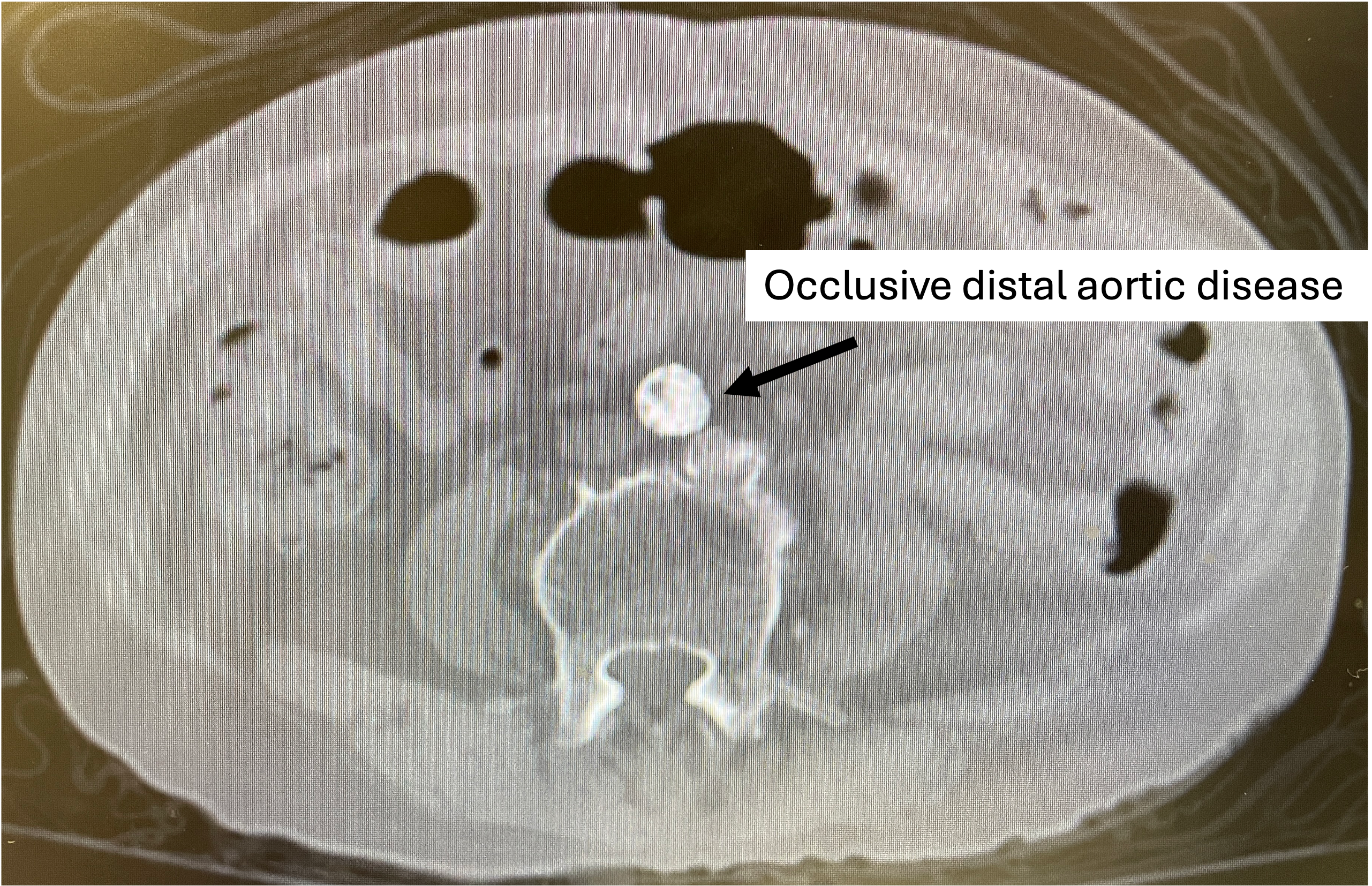
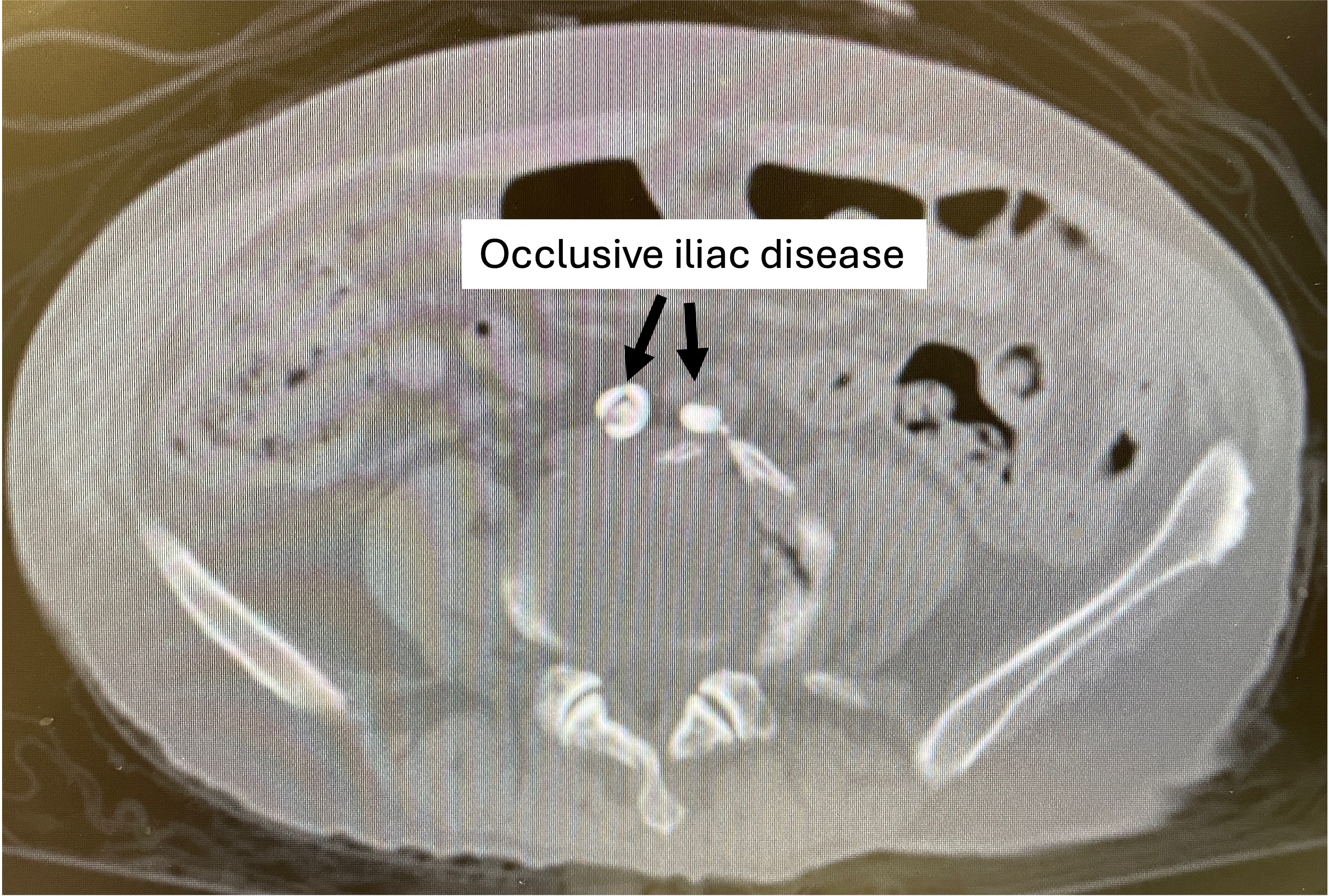
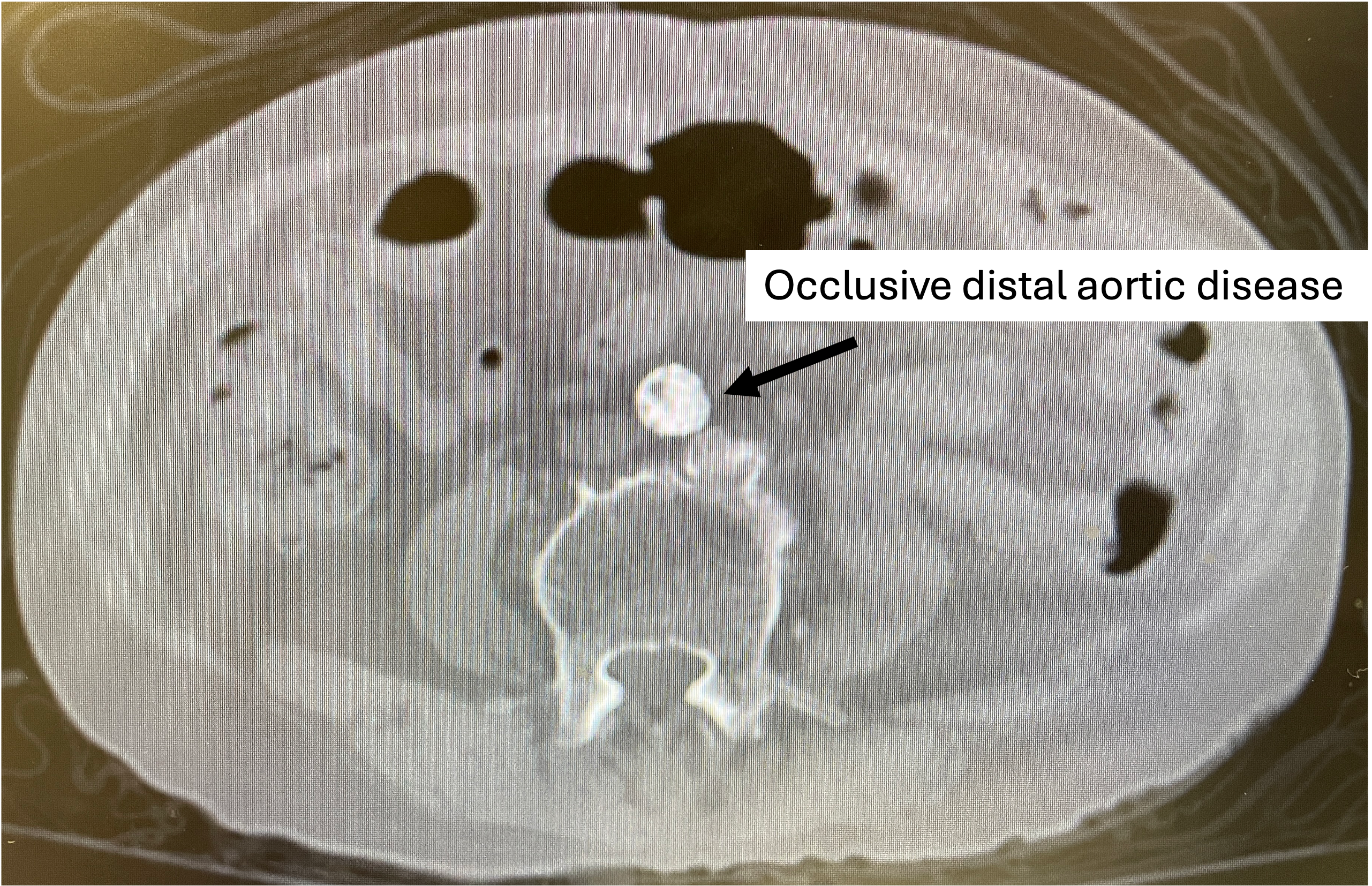
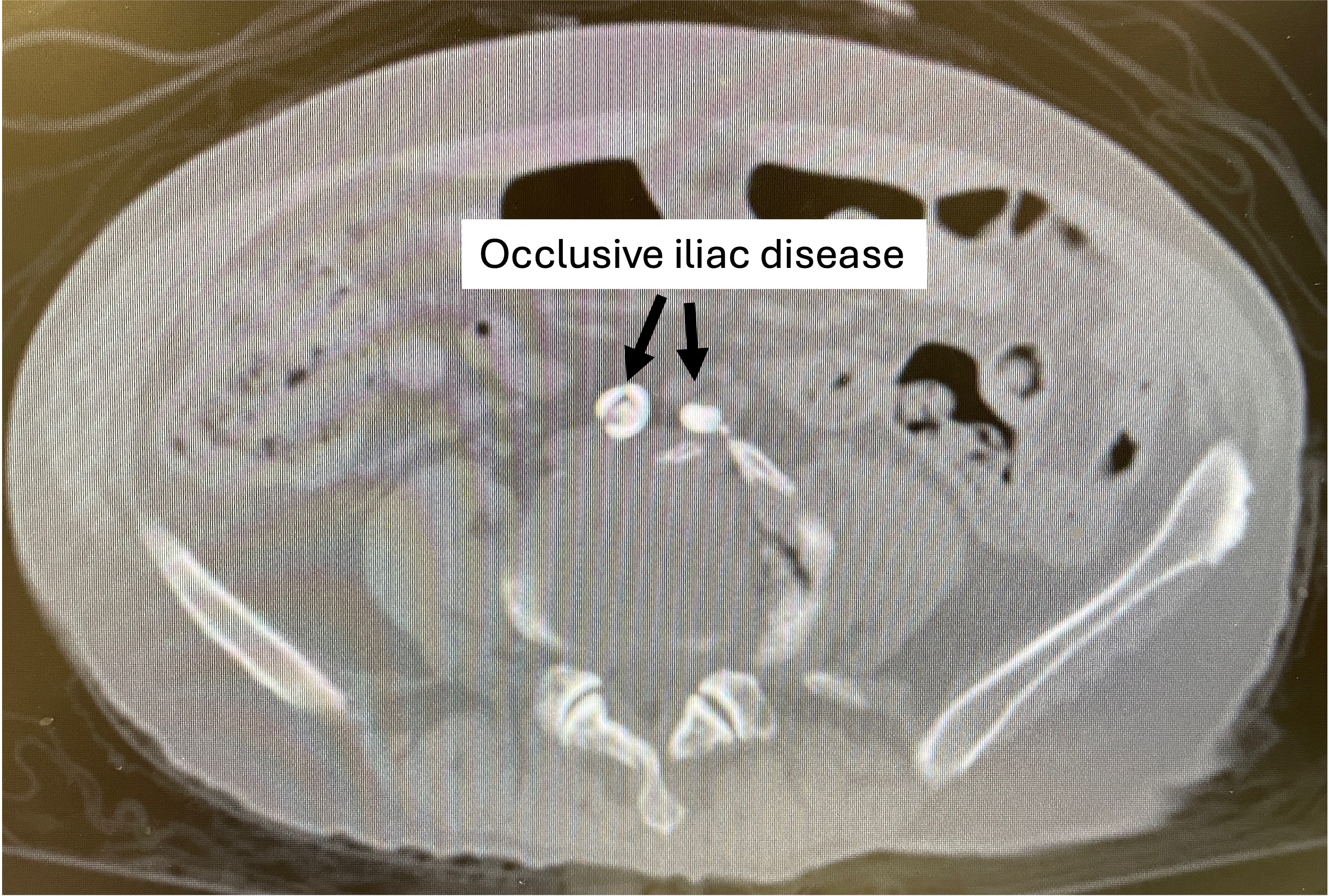
ECG showed RBBB. Haemoglobin was 12g/dL, creatinine 97umol/L, and troponin peaked at 13076ng/L (reference <34). TTE showed severe LV dysfunction (LVEF 25%) with preserved RV function and moderate functional mitral regurgitation. After a period of medical therapy, cardiac MRI showed LVEF improved to 40% with evidence of a previous infarct but viable myocardium. CT showed porcelain aorta and severe aortoiliac disease with occlusions in the infrarenal aorta and bilateral common iliac arteries.
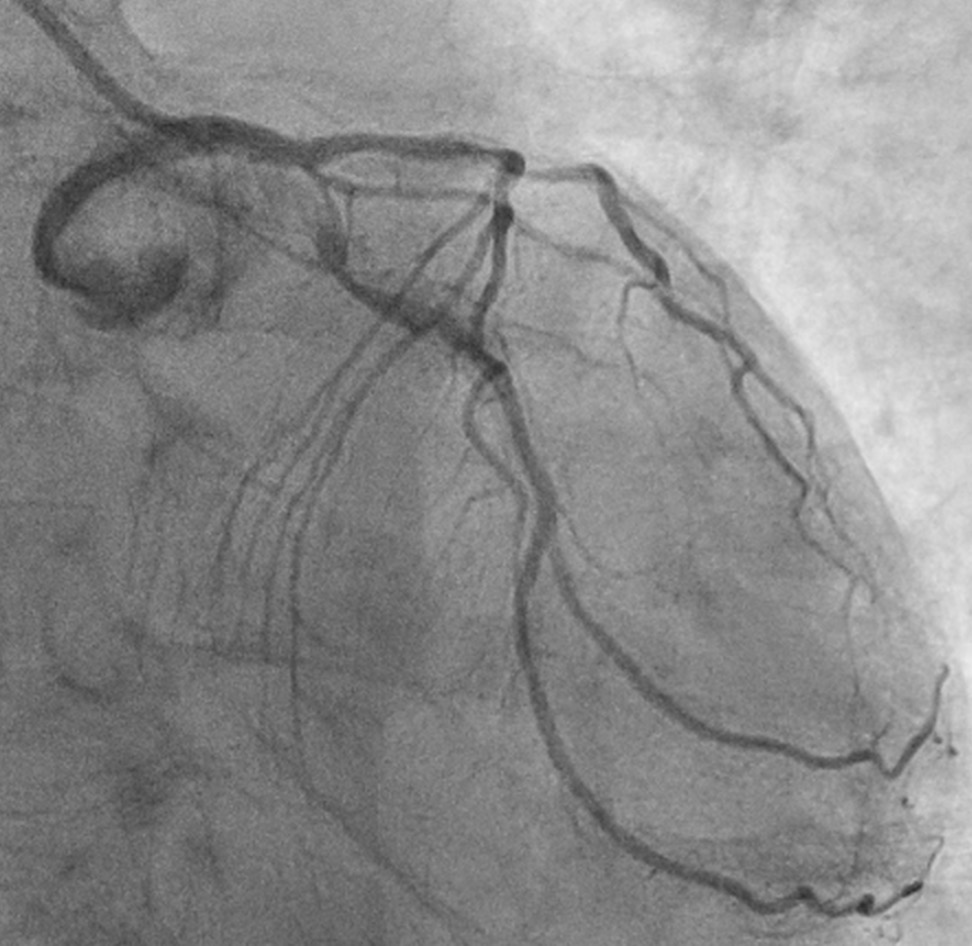
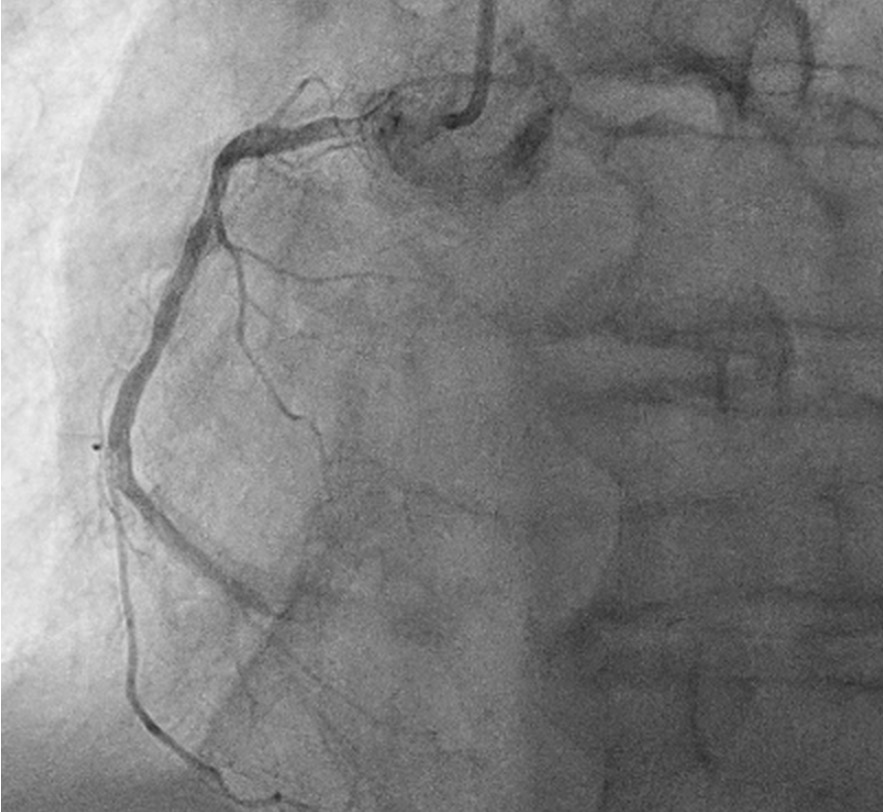
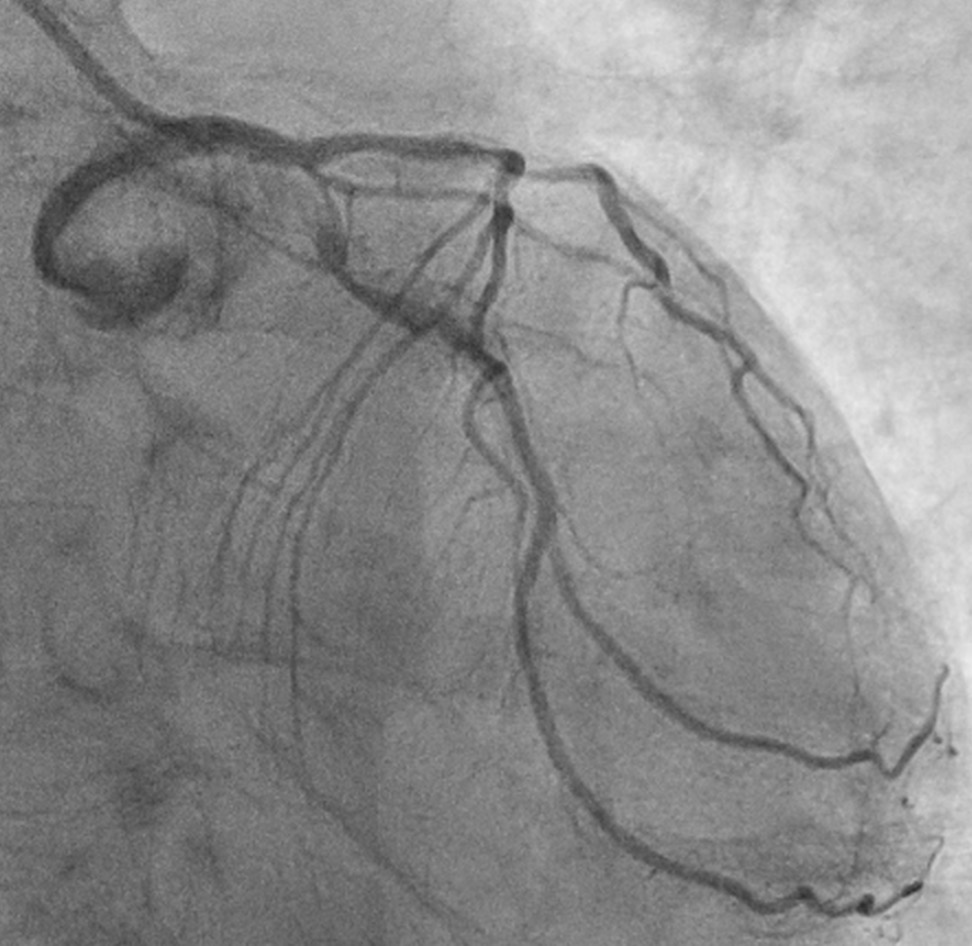
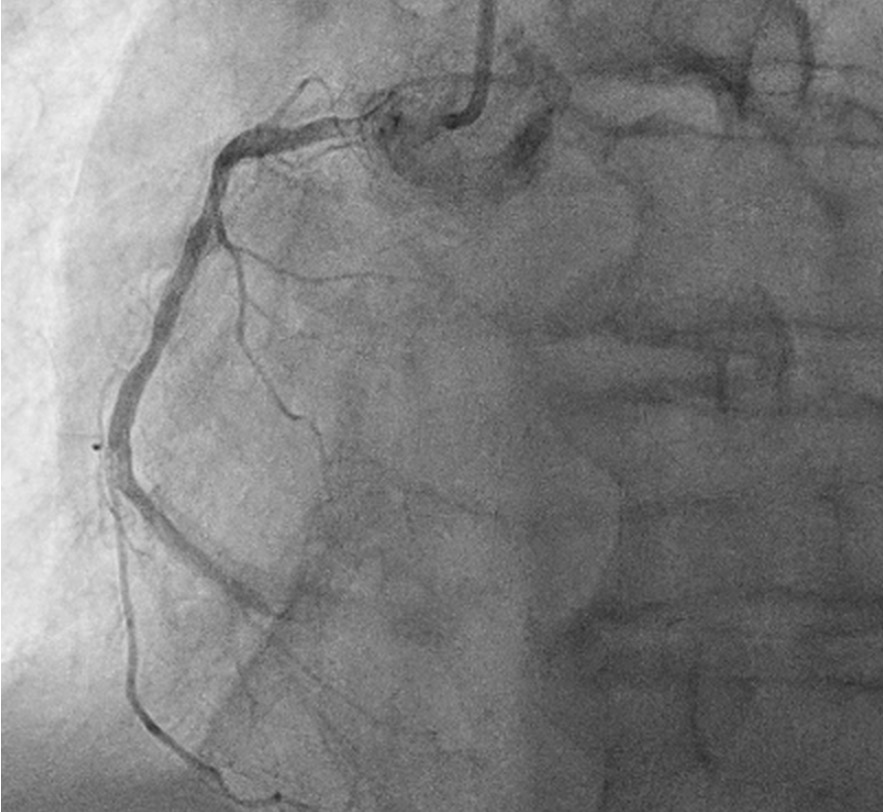
Relevant Catheterization Findings
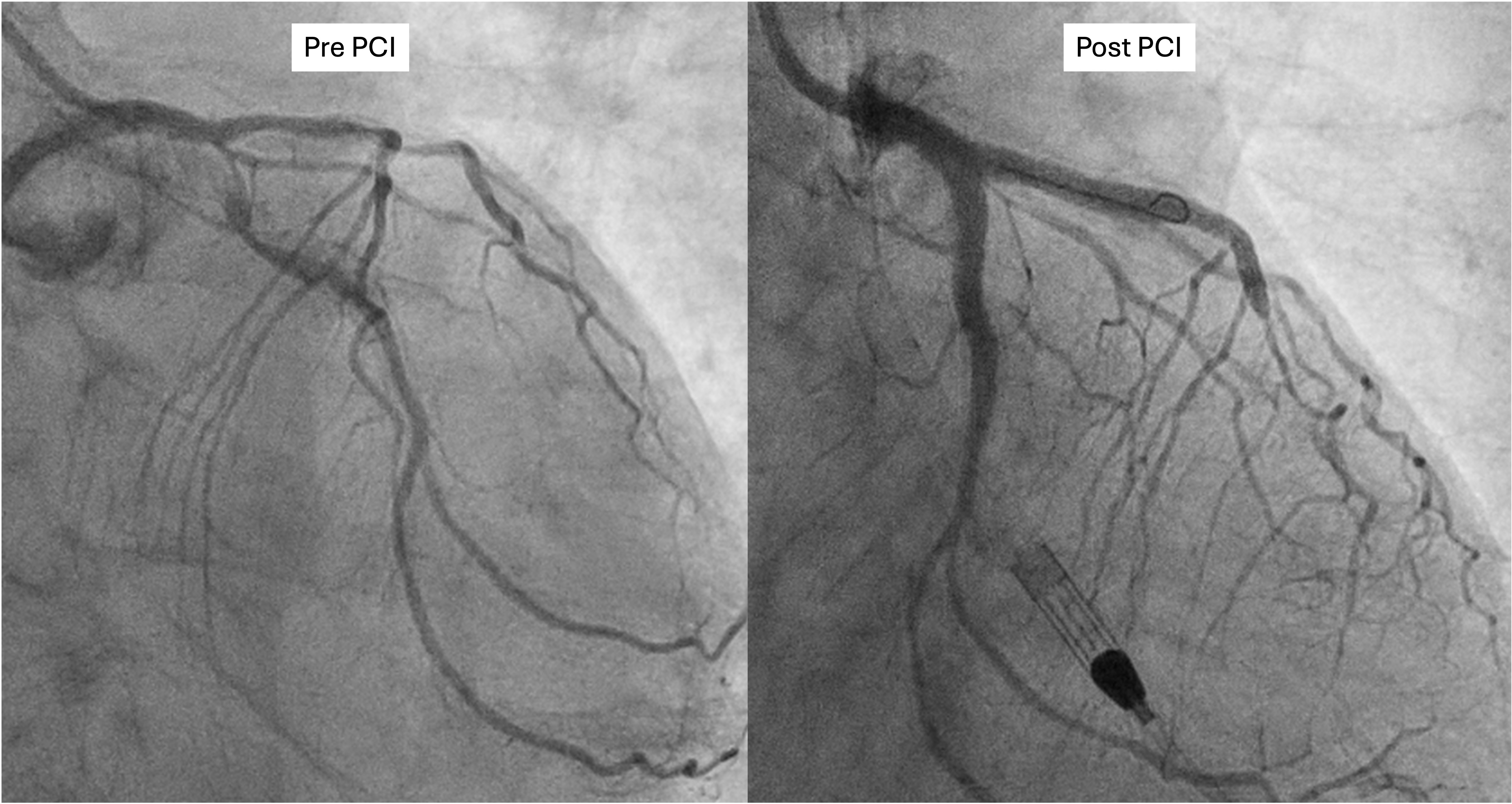
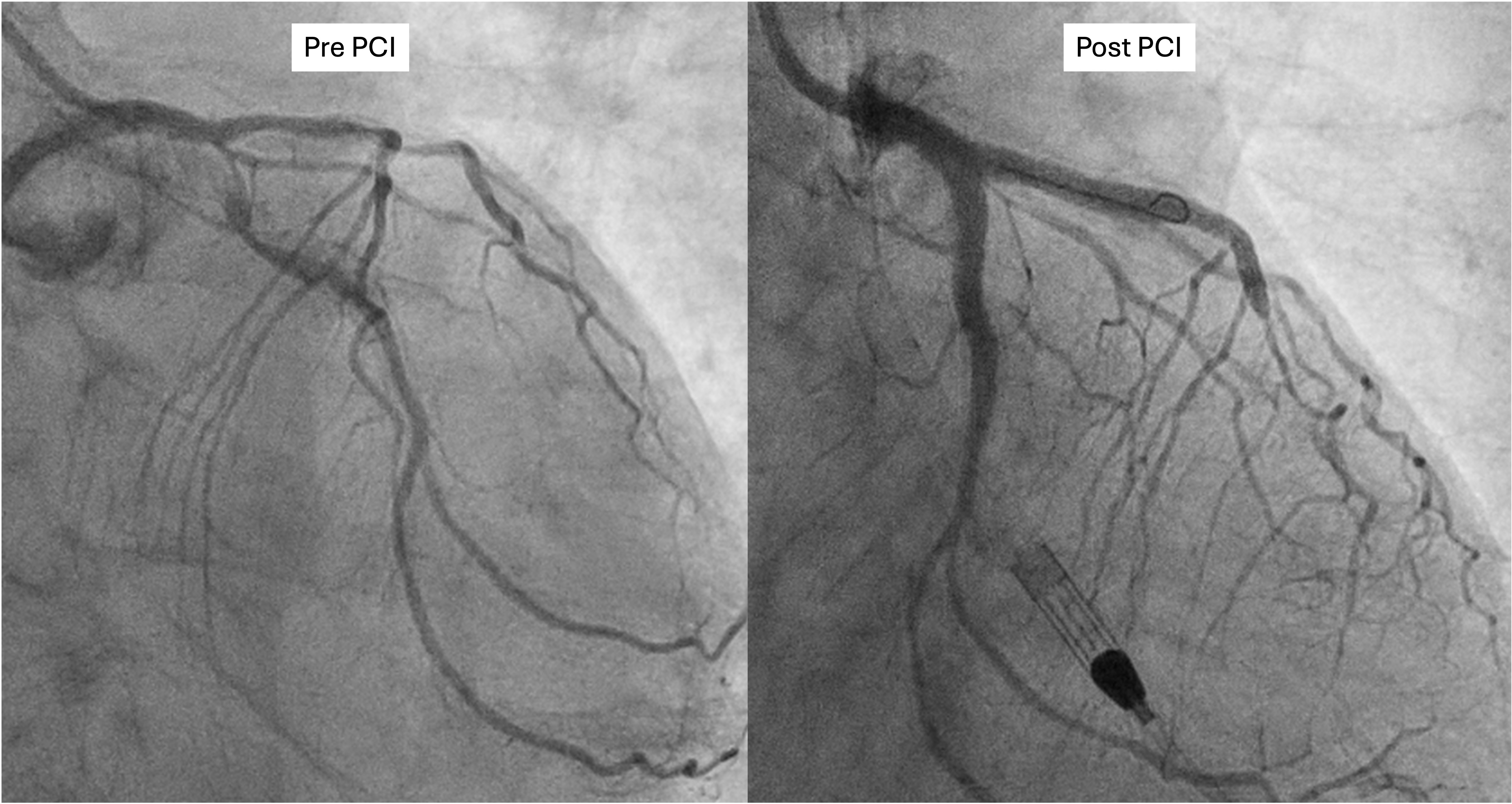
This confirmed severe calcific triple vessel disease. Severe mid LAD diagonal bifurcation stenosis (Medina 1,1,1). Severe LCx ostial and mid stenoses with large ostial calcific nodule. Severe ostial RCA stenosis and distal RCA CTO receiving collateral supply from the septal perforators. CABG was declined due to high surgical risk. After extensive discussions with the patient, his family, and the Vascular Surgical team, high risk vascular and coronary interventions were undertaken.


Interventional Management
Procedural Step
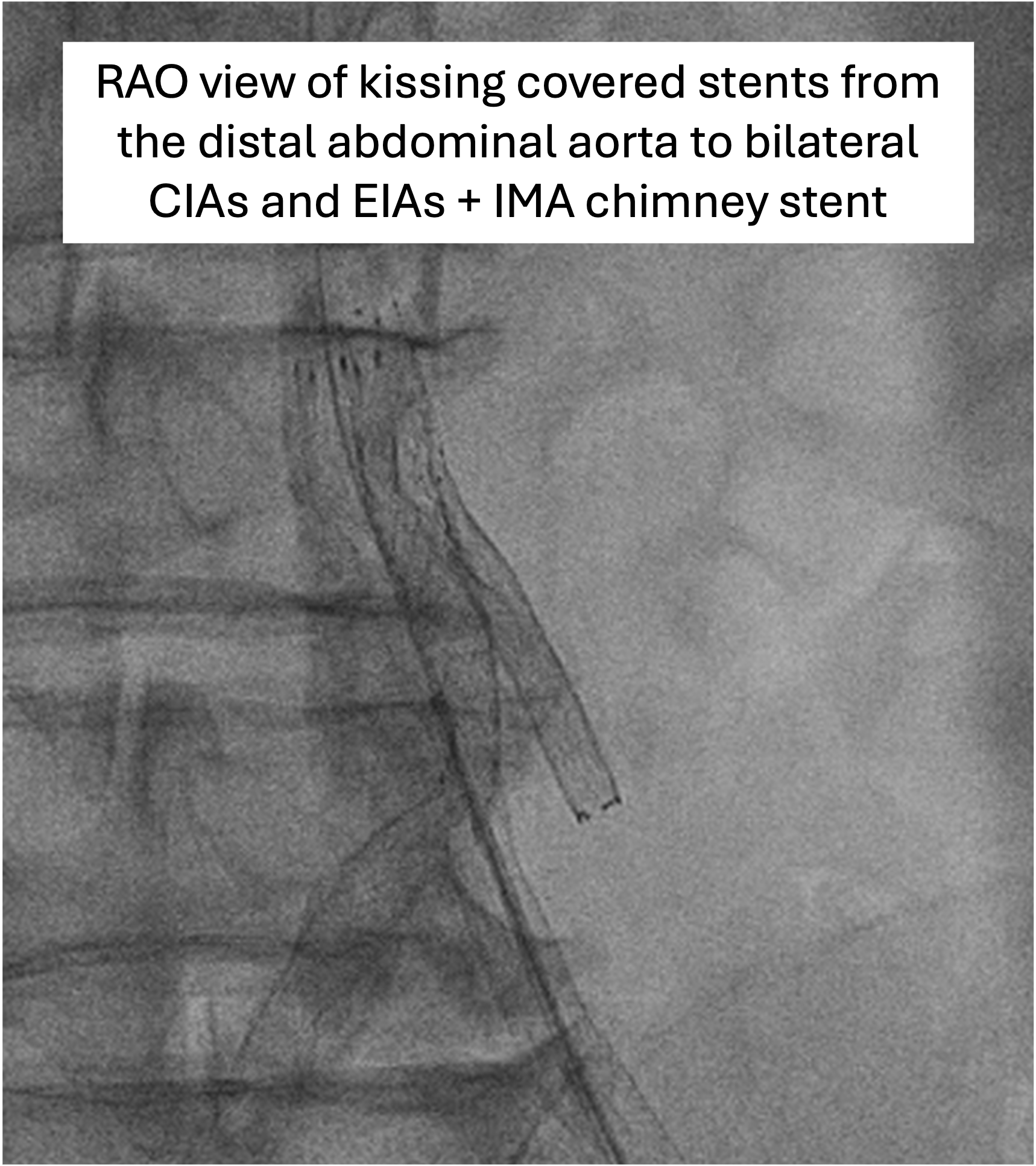
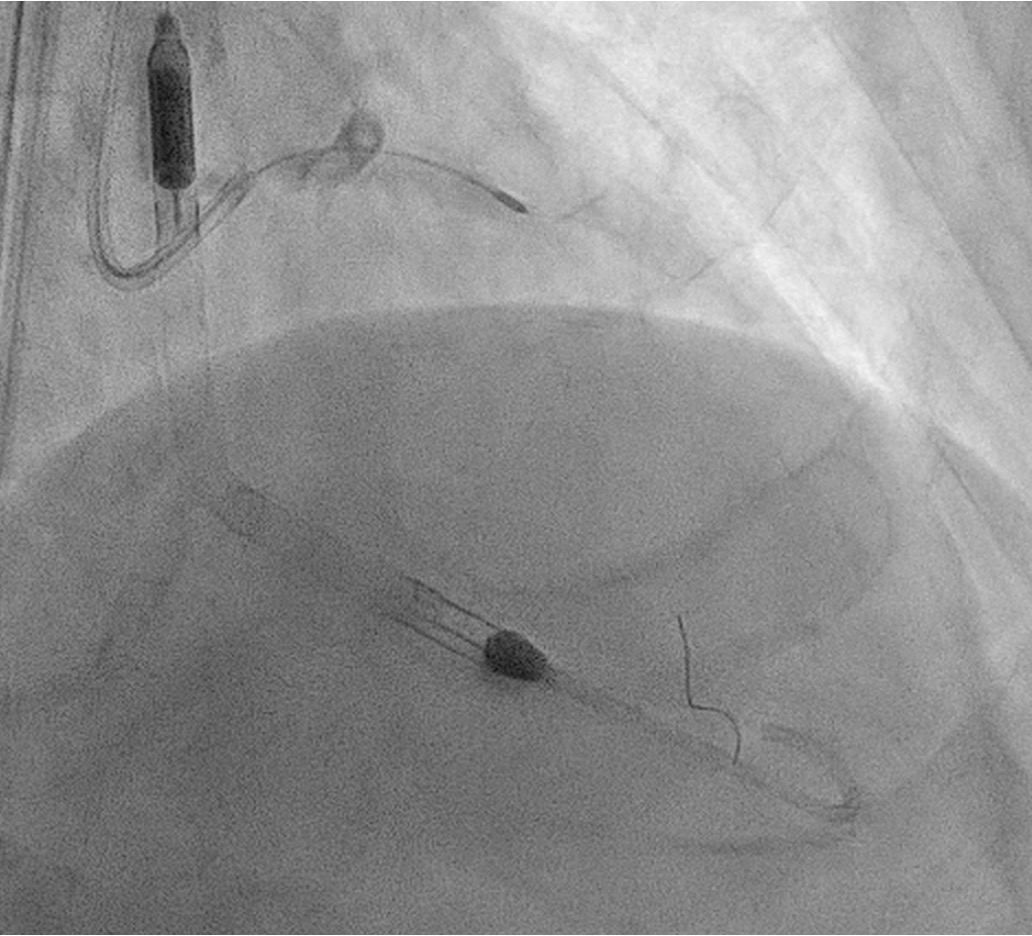
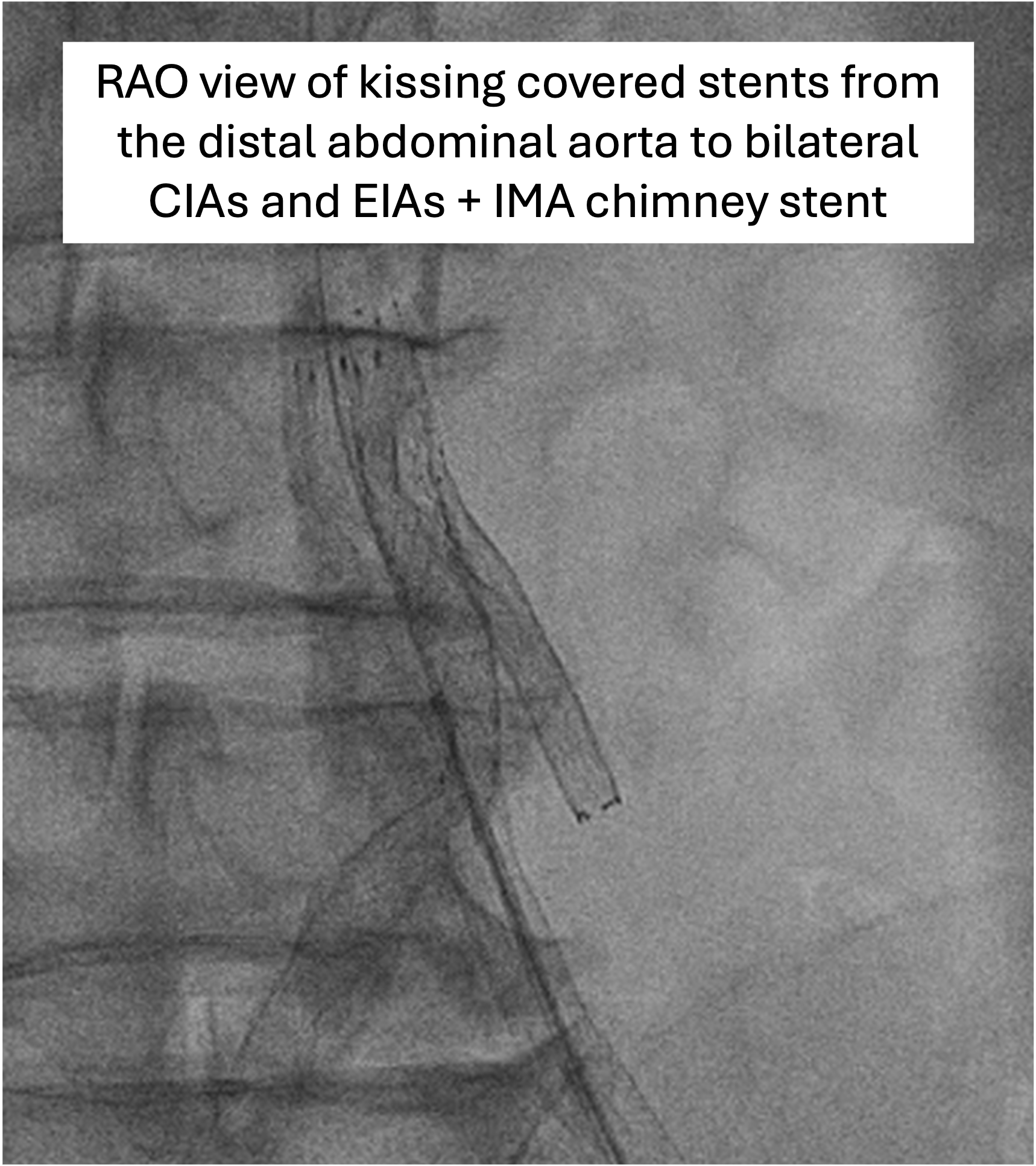
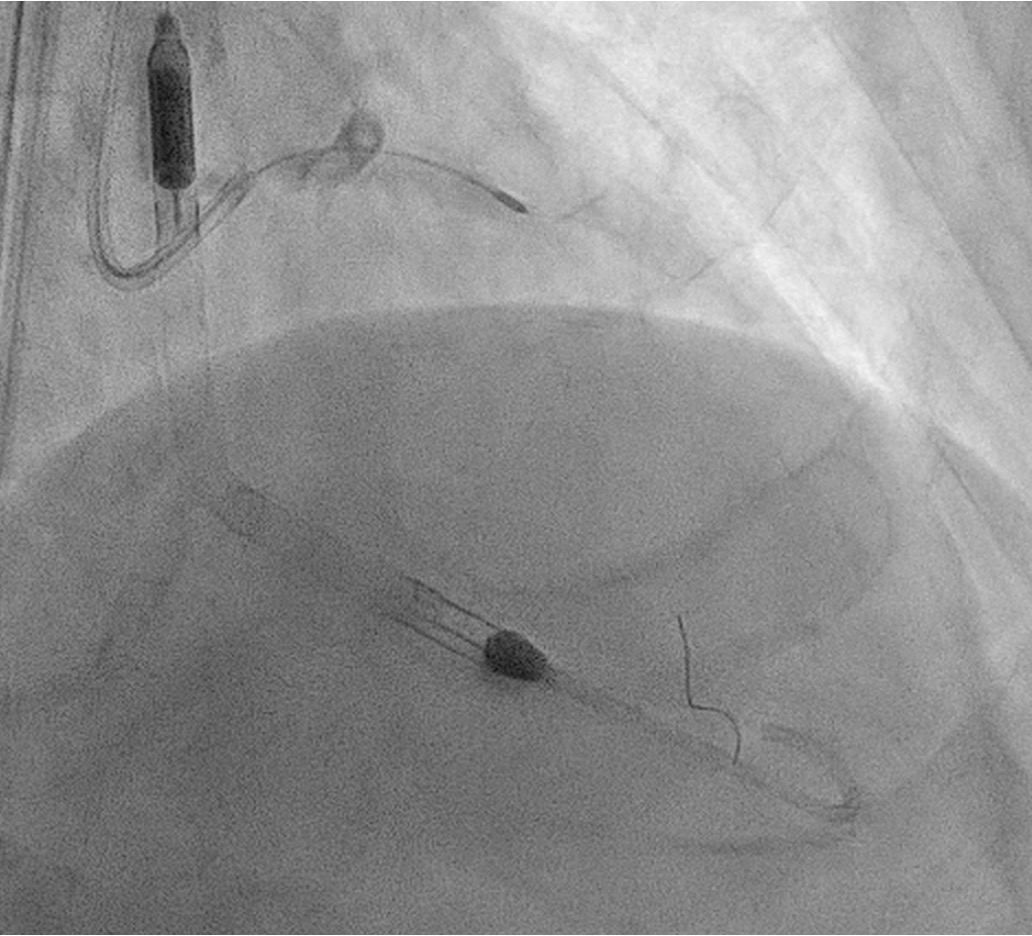
The Vascular team performed aortoiliac revascularisation to concurrently treat his peripheral vascular disease and allow for femoral access for CHIP. Kissing covered stents were placed from the abdominal aorta to bilateral CIAs and EIAs using the “pave and crack” technique with chimney stenting to the IMA. After recovery, single access for Impella CP supported high-risk PCI (SHiP) was performed via the left femoral artery with a 7F sheath through the 14F Impella sheath. Intervention began with the LAD using rotational atherectomy (1.25mm burr) but led to hemodynamic instability despite Impella support, requiring emergency intubation and dopamine infusion. Significant blood loss was noted from the SHiP access due to the inadvertent migration of the PCI sheath proximally, and addressed by repositioning the sheath and transfusion. Once stabilised, the LAD, diagonal, and LCx arteries were treated with rotational atherectomy (1.25mm burr). The LCx had follow up orbital atherectomy, and scoring balloon angioplasty for a large ostial calcific nodule. The left main stem bifurcation was treated with drug eluting stents using OCT guided nano crush technique (3.5/28mm LMS-LAD, 3.5/28mm LCx). The first diagonal and mid LCx were treated with drug eluting balloons (2.5/30mm, 2.5/20mm). Final POT was performed in the LMS (4.0/8mm non-compliant at 18atm). Final OCT and angiography showed satisfactory result with TIMI 3 flow.
Case Summary
This case illustrates the successful integration of the Vascular and Cardiology teams in managing a challenging high-risk patient with complex coronary and peripheral vascular disease. The collaborative approach allowed for effective revascularisation, despite significant challenges, including haemodynamic instability and the need for advanced calcium modification techniques.
