CASE20250822_007
The Unexpected Roadblock
By Hendrianus Hendrianus, Sang-Wook Kim
Presenter
Hendrianus Hendrianus
Authors
Hendrianus Hendrianus1, Sang-Wook Kim1
Affiliation
Heart and Brain Hospital, Chung-Ang University Medical Center, Indonesia1
View Study Report
CASE20250822_007
ACS/AMI - ACS/AMI
The Unexpected Roadblock
Hendrianus Hendrianus1, Sang-Wook Kim1
Heart and Brain Hospital, Chung-Ang University Medical Center, Indonesia1
Clinical Information
Relevant Clinical History and Physical Exam
A 67-year-old man arrived at the emergency department complaining of continuous chest discomfort and shortness of breath for the past two days, with a marked worsening of both symptoms during the two hours prior to presentation.
Relevant Test Results Prior to Catheterization
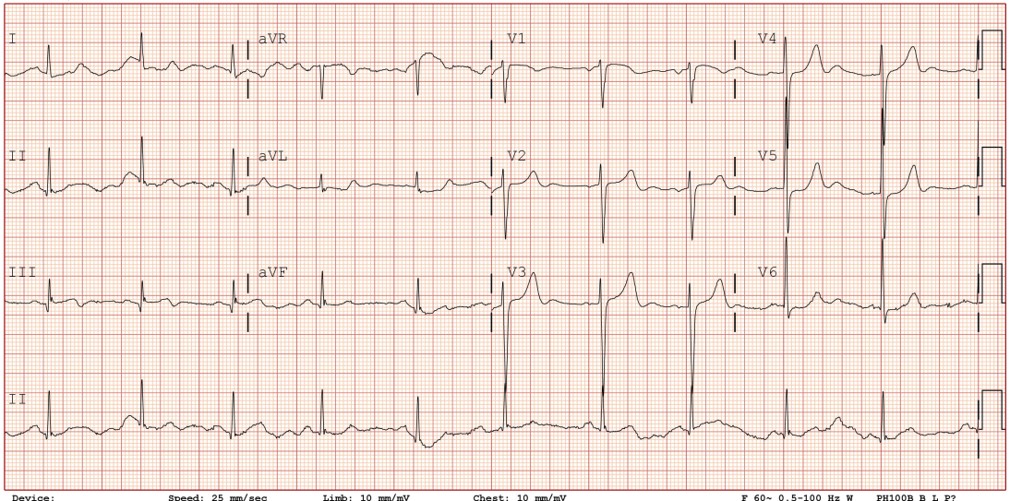
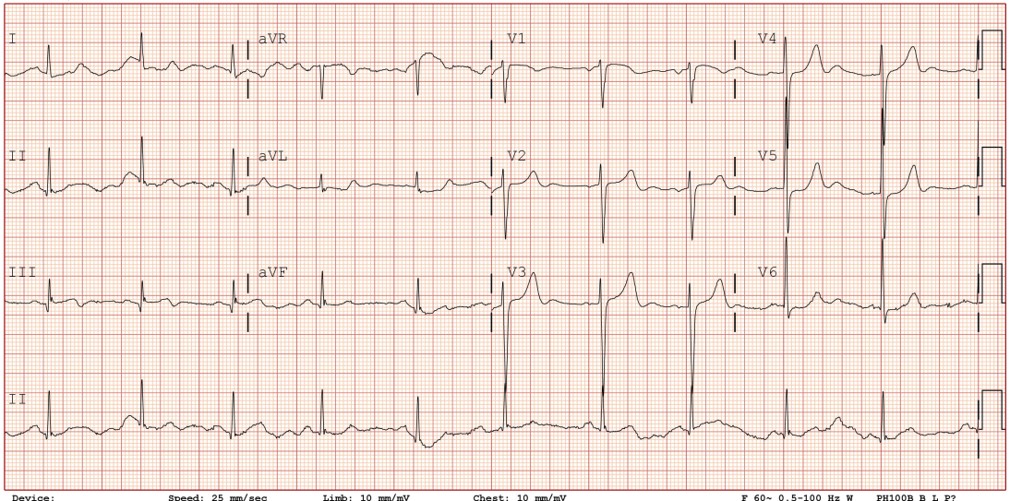
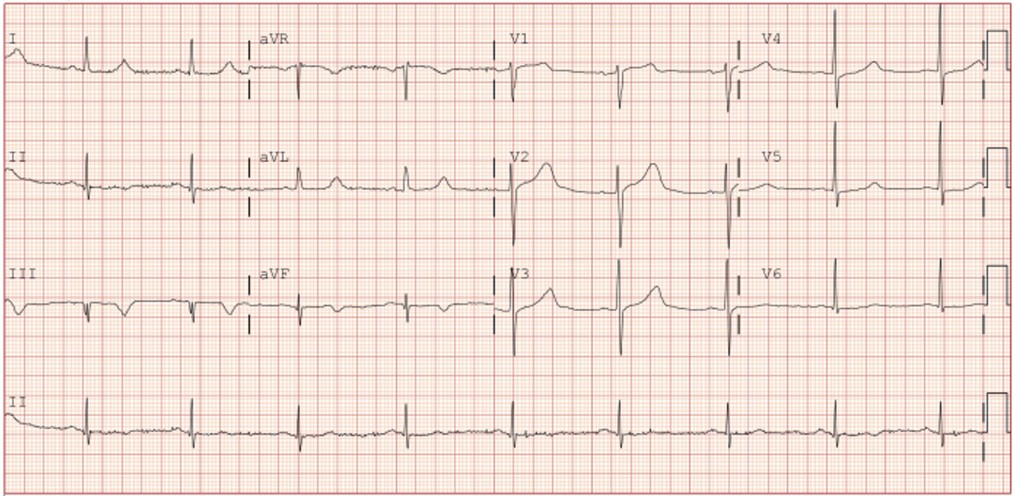
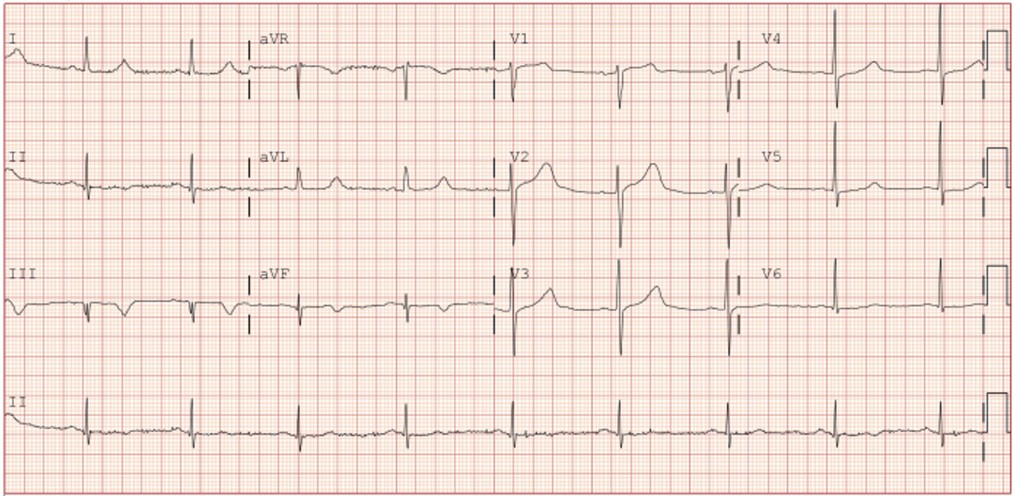
ECG showed a biphasic T wave in lead III without other significant ST-segment changes.
Relevant Catheterization Findings
Emergent coronary angiography via left distal radial access revealed subtotal occlusion of the distal LCX and total occlusion of the RCA with well-developed collaterals—suggesting a chronic total occlusion (CTO).
 DiagnosticCAG1.wmv
DiagnosticCAG1.wmv
 DiagnosticCAG2.wmv
DiagnosticCAG2.wmv
 DiagnosticCAG3.wmv
DiagnosticCAG3.wmv
Interventional Management
Procedural Step
The LCX was presumed the culprit and was treated with a drug-coated balloon (DCB). Despite successful treatment, the patient still has chest discomfort. Echocardiogram showed inferolateral hypokinesis. Re-evaluation led to RCA wiring, which proved unexpectedly easy—raising concerns about subintimal passage or the possibility of an acute thrombotic occlusion rather than CTO. IVUS confirmed wire position within the true lumen and revealing plaque rupture and thrombus, thereby establishing the RCA as the true culprit lesion. Prompt PCI was performed: balloon pre-dilation followed by deployment of a drug-eluting stent. IVUS ensured optimal stent expansion and confirmed absence of dissection or malapposition. Post-procedurally, the patient stabilized, and follow-up ECG showed T-wave inversion in the inferior leads, consistent with evolving infarction in the RCA territory.
 RCA_IVUS.wmv
RCA_IVUS.wmv
 Final CAG after PCI RCA.wmv
Final CAG after PCI RCA.wmv
Case Summary
Collateral flow to an acutely thrombosed artery may mimic a CTO, leading to misidentification and mistreatment of the true culprit lesion. Re-evaluation and dynamic decision-making are essential. In this case, IVUS proved critical at two key points: (1) confirming wire position within the true lumen, and (2) revealing thrombus and plaque rupture—distinguishing an acute thrombotic occlusion from a presumed CTO in the RCA.
