CASE20250822_014
Intraperitoneal Bleeding: An Unusual Complication During PCI
By Michael Lo Jianhui, Simon Lo
Presenter
Michael Lo Jianhui
Authors
Michael Lo Jianhui1, Simon Lo2
Affiliation
Royal Surrey Hospital, United Kingdom1, Gleneagles Hospital Penang, Malaysia2
View Study Report
CASE20250822_014
Complication Management - Complication Management
Intraperitoneal Bleeding: An Unusual Complication During PCI
Michael Lo Jianhui1, Simon Lo2
Royal Surrey Hospital, United Kingdom1, Gleneagles Hospital Penang, Malaysia2
Clinical Information
Relevant Clinical History and Physical Exam
A 75-year-old Chinese male presented with increasing exertional dyspnoea with chest discomfort for 6 months in 2024. He had PCI to his LAD in 2006, and his follow-up was in a public hospital. Past medical history included hypertension, hyperlipidaemia, stage 1 CKD and a 6 month history of bullous pemphigoid. Regular medications included Aspirin 100mg od, Atorvastatin 40 mg od, Perindopril 4 mg od, Chlorothiazide 25 mg od, Prednisolone 5 mg od. Physical examination revealed a pansystolic murmur.


Relevant Test Results Prior to Catheterization
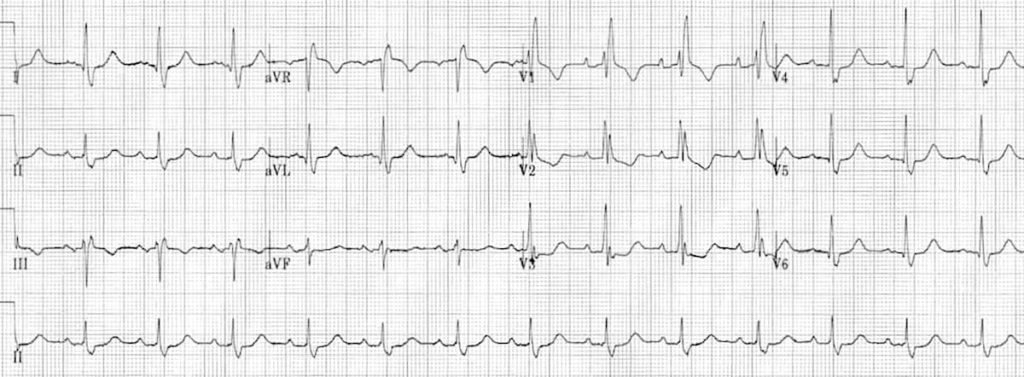
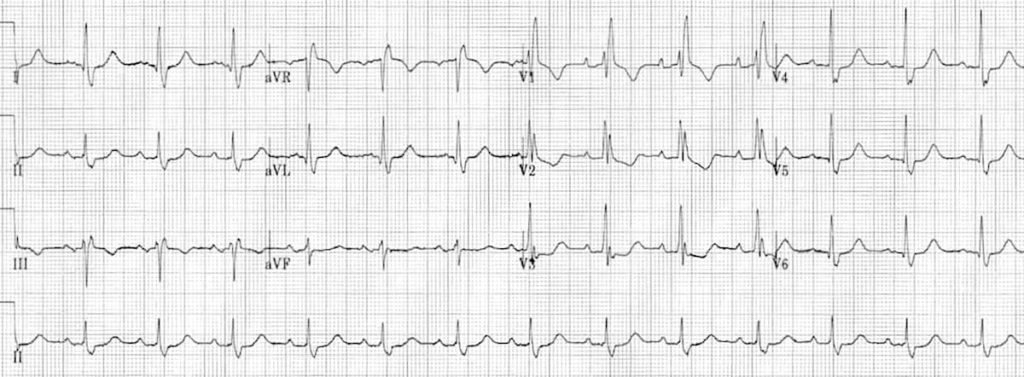
Lab data: HbA1c 6.2%; Creatinine 102 mmol/L; eGFR 63.1 mL/min/1.73m2; TC 5.4 mmol/L; LDL 2.9 mmol/L; HDL 1.7 mmol/L; Triglycerides 1.7 mmol/LECG: SR with RBBBECHO: LV normal size, borderline LVH, EF 65%, mild MR
Relevant Catheterization Findings
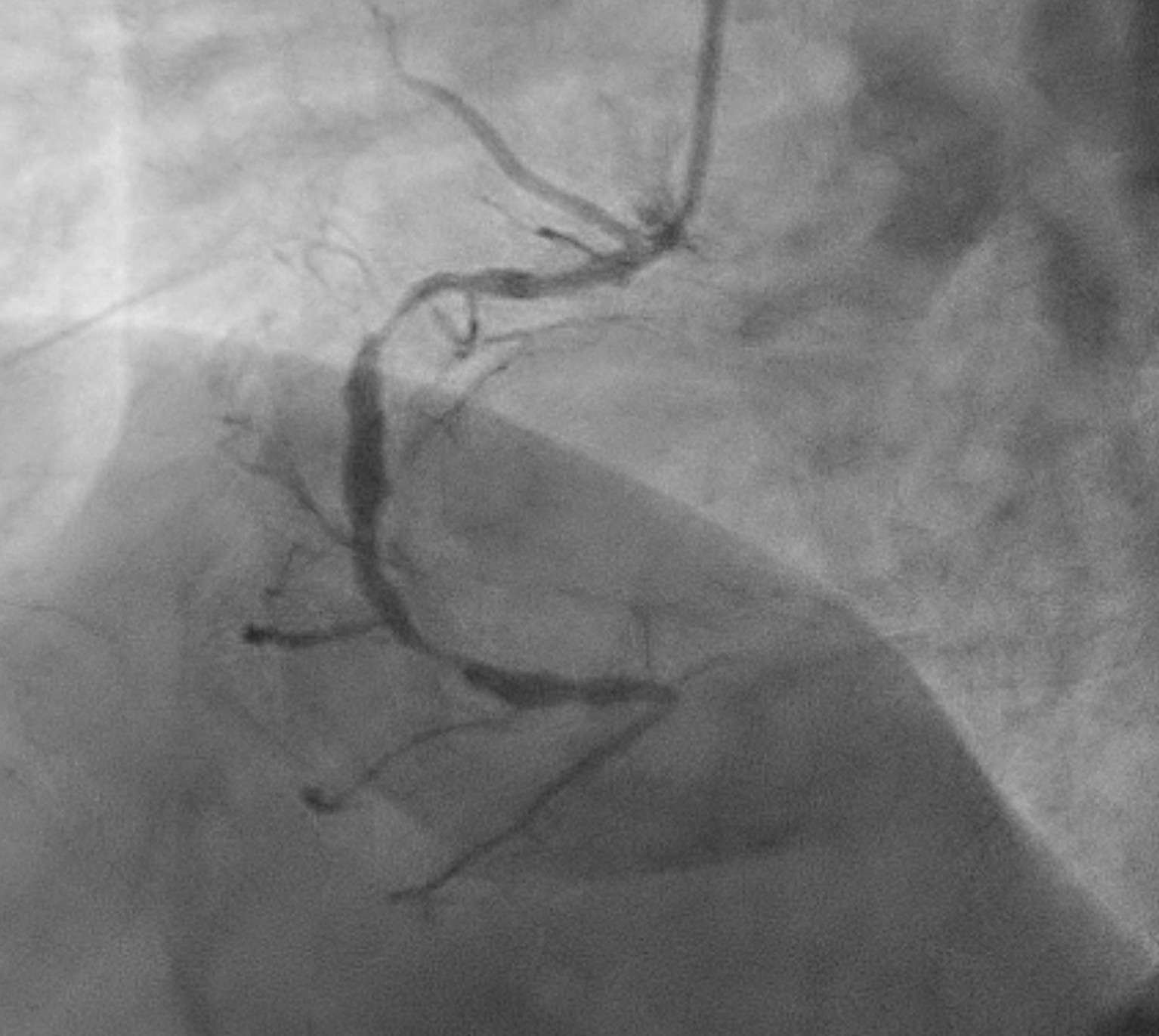
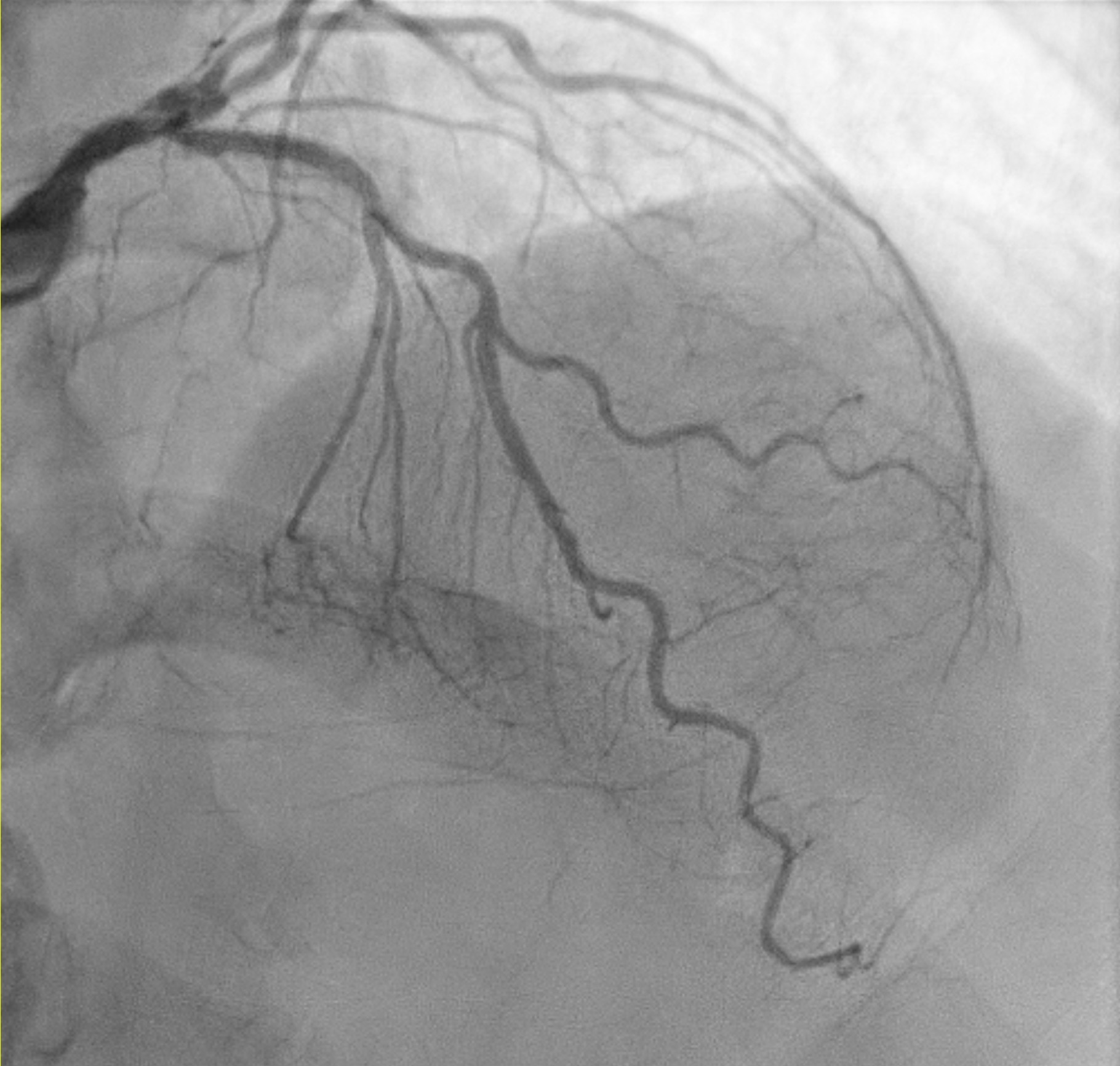
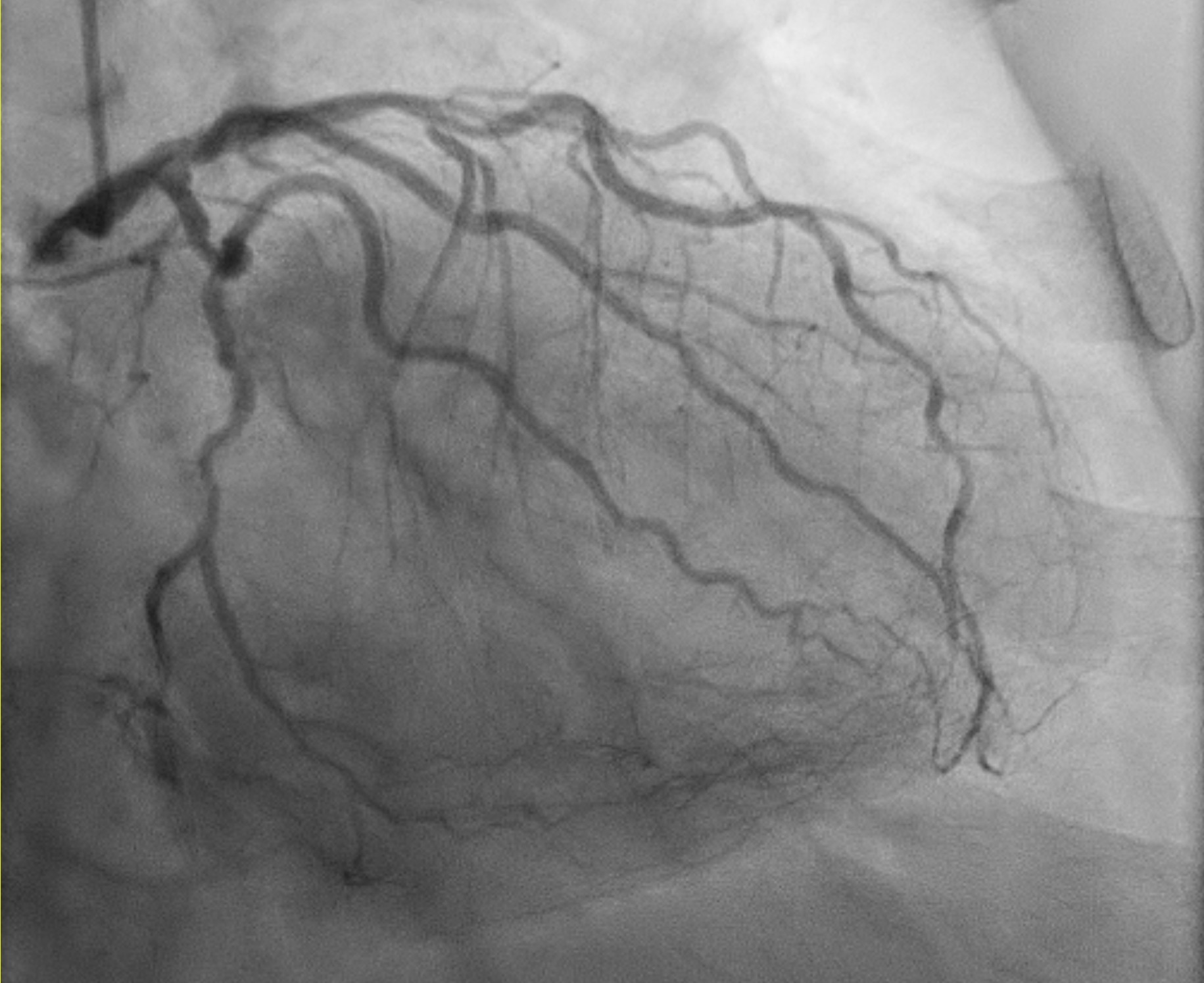
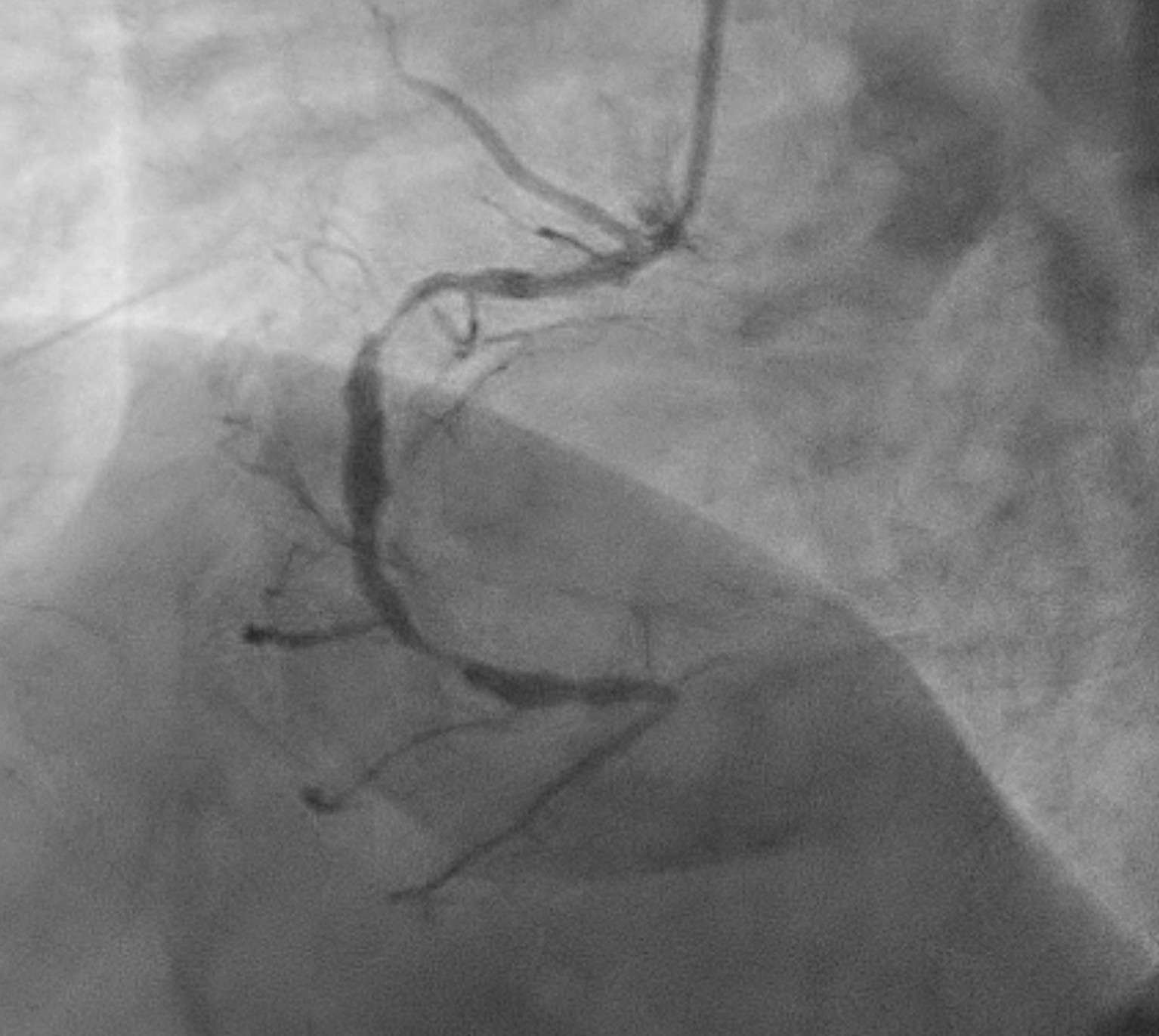
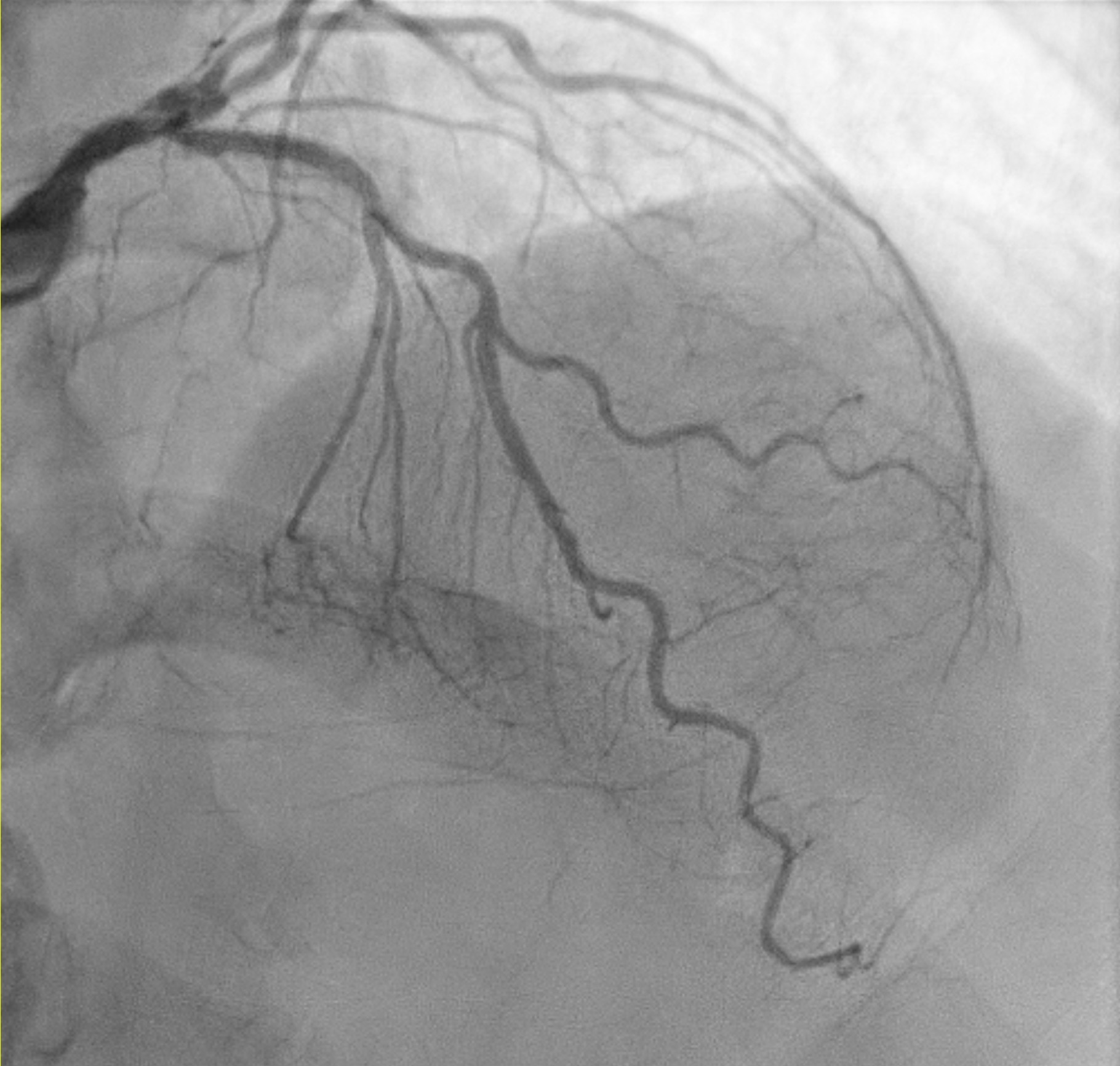
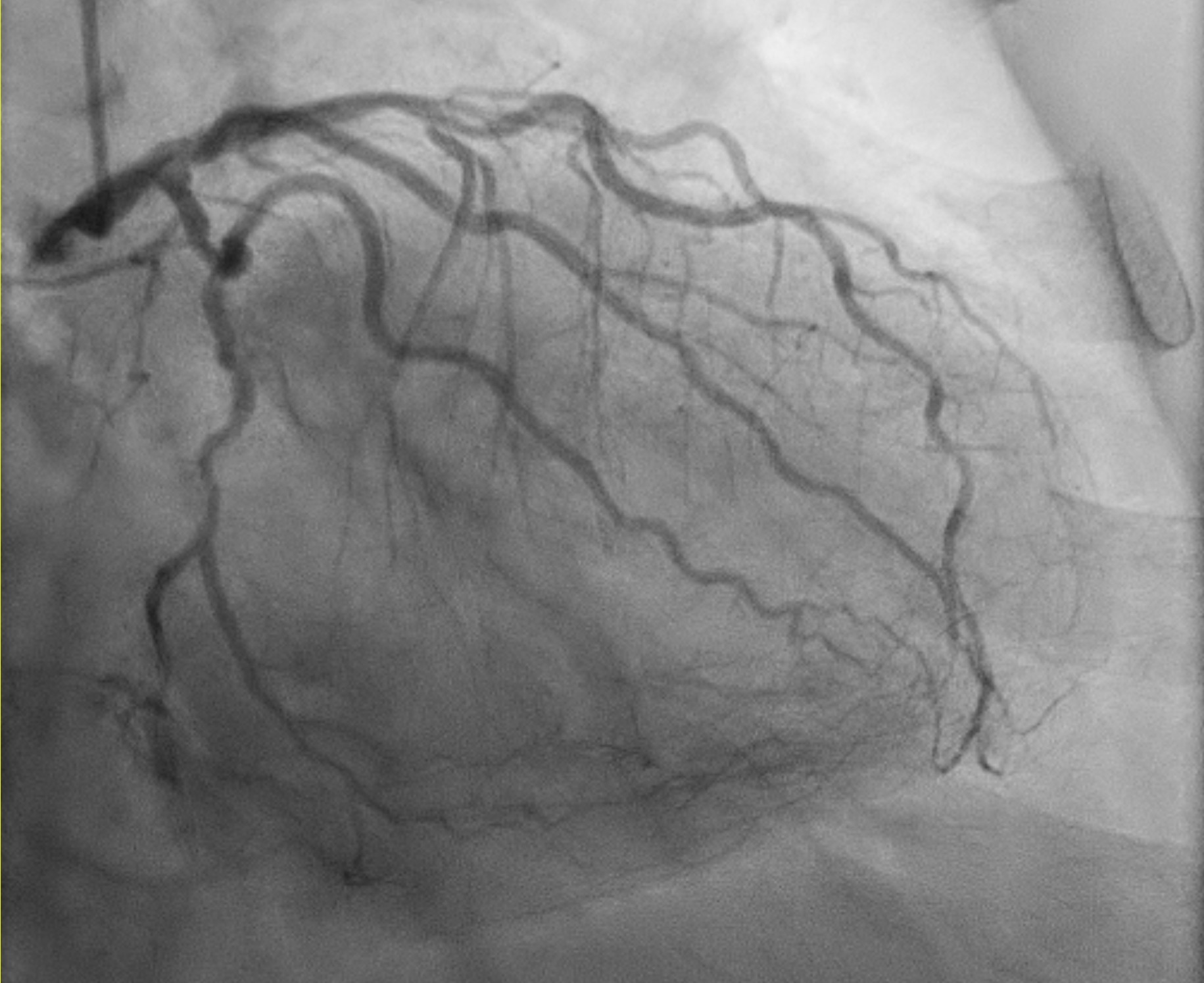
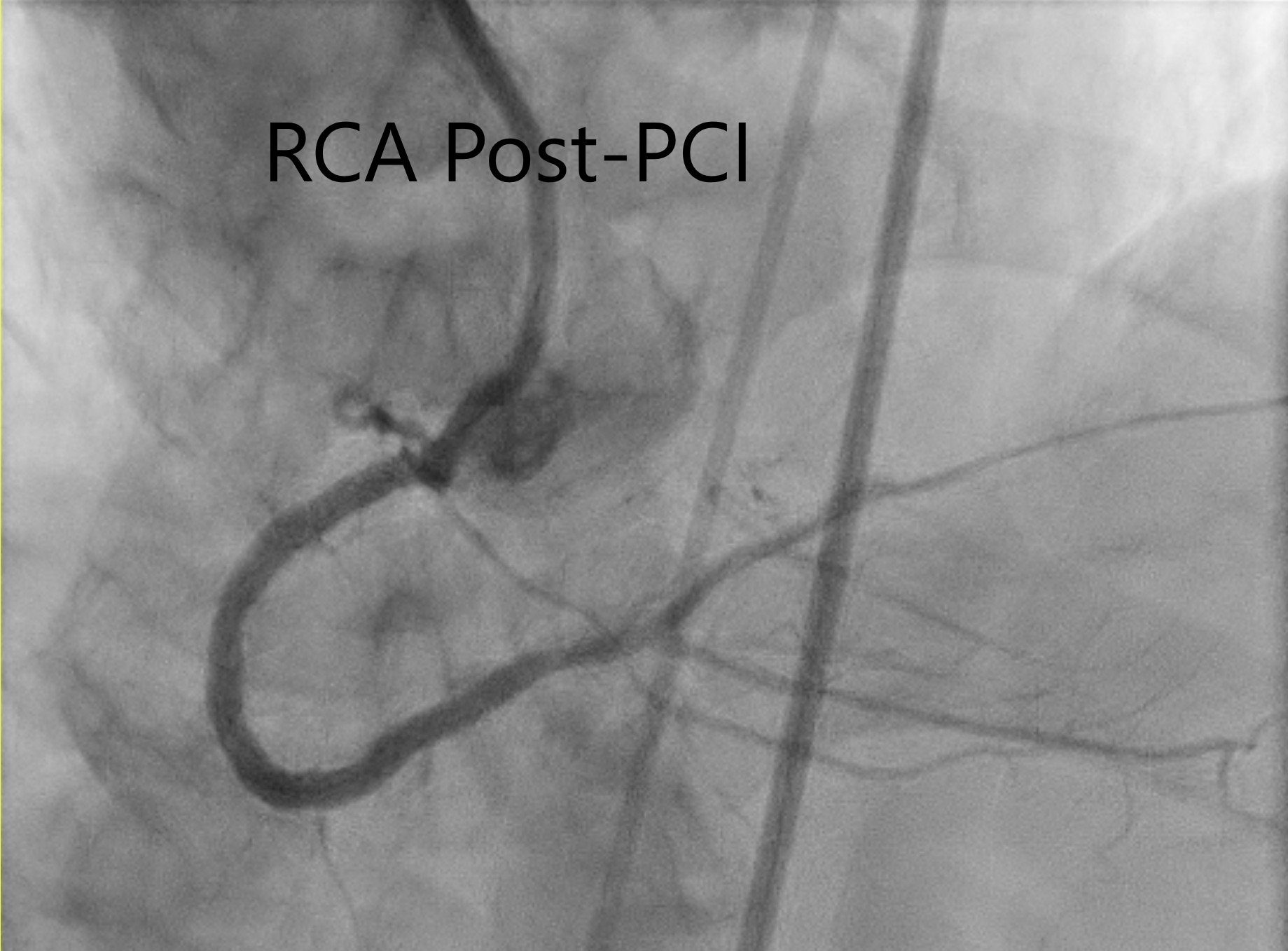
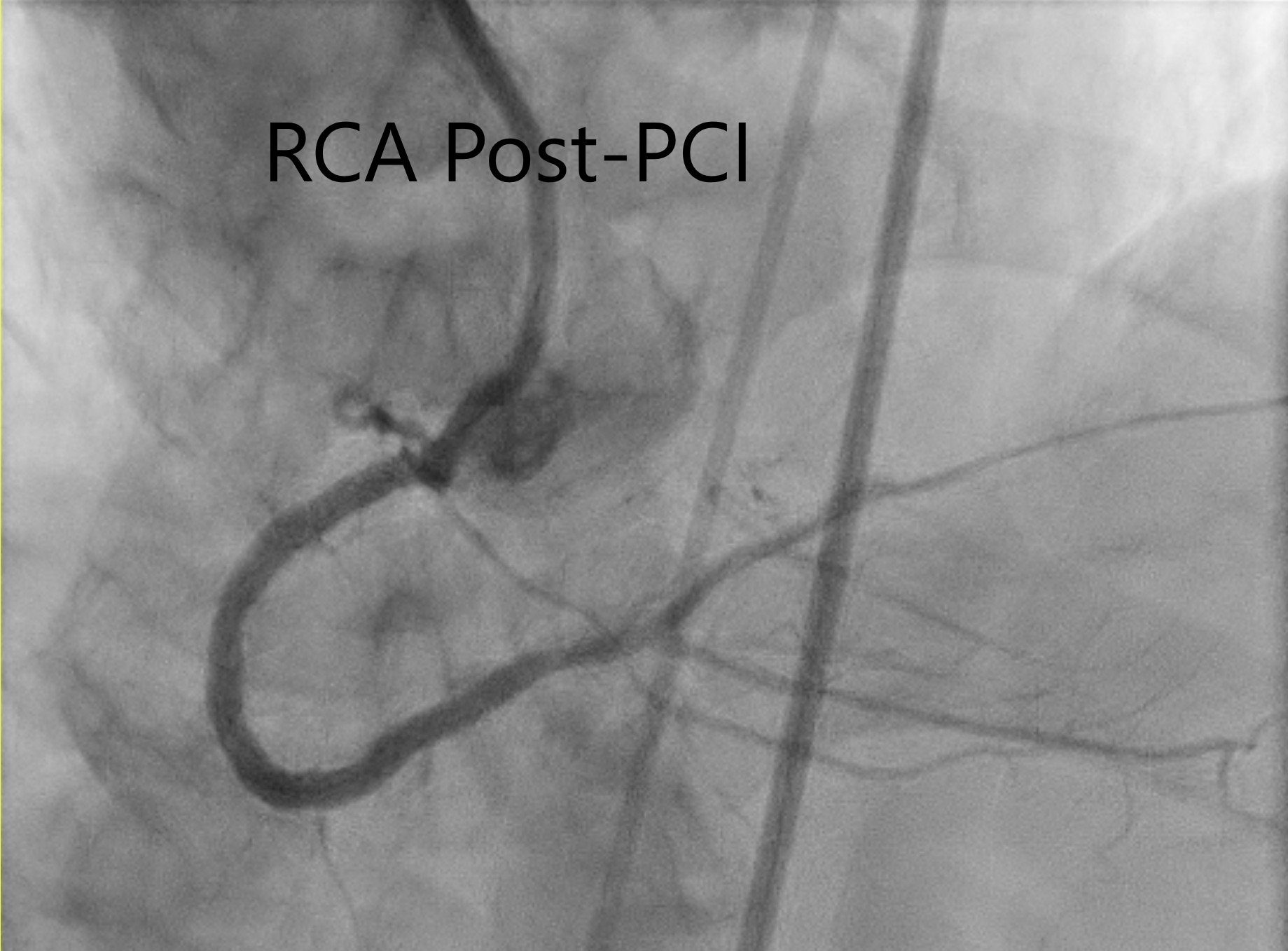
TRA diagnostic angiogram (pictures 1-3) showed mild distal LMS. Mild proximal-mid LAD stent <20% ISR and distal LAD 50% stenosis. Distal circumflex 50% stenosis. Proximal RCA 90% stenosis, distal 70% (segment 3) and then followed by total occlusion. Distal RCA received collaterals from LCA. Results discussed with patient who agreed for elective angioplasty to RCA.
Interventional Management
Procedural Step
Bifemoral approach. 7F and 5F sheaths in the right and left respectively. Heparin 7000 units. 7F Cordis AL1 GC and 5F APT JL4 DC were inserted with 0.035 J-tip Teflon wire (B Braun). Starting BP 158/72 mmHg. RCA stenoses and CTO were successfully crossed Gaia 3rd wire (Asahi). Distal RCA stented with DES 2.75x34 and ostial-mid RCA stented using DES 3x46mm (iVascular). Immediately after this, 2nd stent was placed. His sBP dropped from 134 to 70 mmHg over 2 minutes. A presumed diagnosis of vasovagal response was made. IV Atropine 0.5 mg bolus, IV Adrenaline 0.5 mg bolus, IV normal saline bolus were given. Immediate echo showed no pericardial effusion. Before sheath removal, the patient developed his BP dropped to 70 mmHg. IV infusion of Noradrenaline given. Bilateral iliac and femoral angiogram showed no evidence of bleeding from the puncture sites. The patient developed distended abdomen. Urgent CT abdominal scan showed a large right sided mesenteric mass with dilated tortuous vessels in keeping with a pseudoaneurysm. A diagnosis of “intraperitoneal arteriovenous malformation bleeding with feeding arteries from SMA” was made.The patient underwent urgent embolization of the bleeding sites using using 7 pushable helical coils: 3 of 4 x 40 mm coils and 4 Vortx Diamond pushable coils (4 x 3.77 mm) (Boston Scientific). Repeat DSA and angiogram 1 minute and 5 minutes later showed no more bleeding.
 Video 1 DSA. Bleeding from a branch of superior messneteric artery.avi
Video 1 DSA. Bleeding from a branch of superior messneteric artery.avi
 Video 4 DSA. No more bleeding.avi
Video 4 DSA. No more bleeding.avi
Case Summary
Haemoperitoneum from a superior mesenteric arteriovenous malformation during PCI is extraordinarily rare. The usualcomplication with femoral access remains retroperitoneal haemorrhage, whereas intraperitoneal haemorrhage essentially only occurssecondary to unusual circumstances like this patient’s visceral arteriovenous malformation. ACT abdominal angiography can be life-saving as it provides rapid information forits diagnosis and guide its subsequent therapy.
