CASE20250903_004
When Both Caps Are Ambiguous: Complex PCI for RCA CTO
By Soo Yeon An
Presenter
Soo Yeon An
Authors
Soo Yeon An1
Affiliation
Asan Medical Center, Korea (Republic of)1
View Study Report
CASE20250903_004
Complex PCI - CTO
When Both Caps Are Ambiguous: Complex PCI for RCA CTO
Soo Yeon An1
Asan Medical Center, Korea (Republic of)1
Clinical Information
Relevant Clinical History and Physical Exam
A 58-year-old male with a history of hypertension and dyslipidemia presented with CCS Class III angina persisting for six months. His past medical history was significant for percutaneous coronary intervention (PCI) performed nine years prior, involving a distal right coronary artery (RCA) lesion and a left anterior descending (LAD) chronic total occlusion (CTO). Current medications included aspirin, carvedilol, nicorandil, and statins. Physical examination and vital signs were unremarkable.
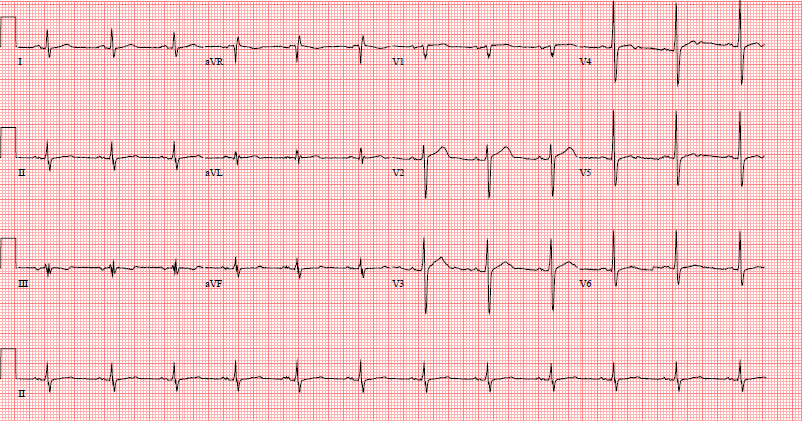
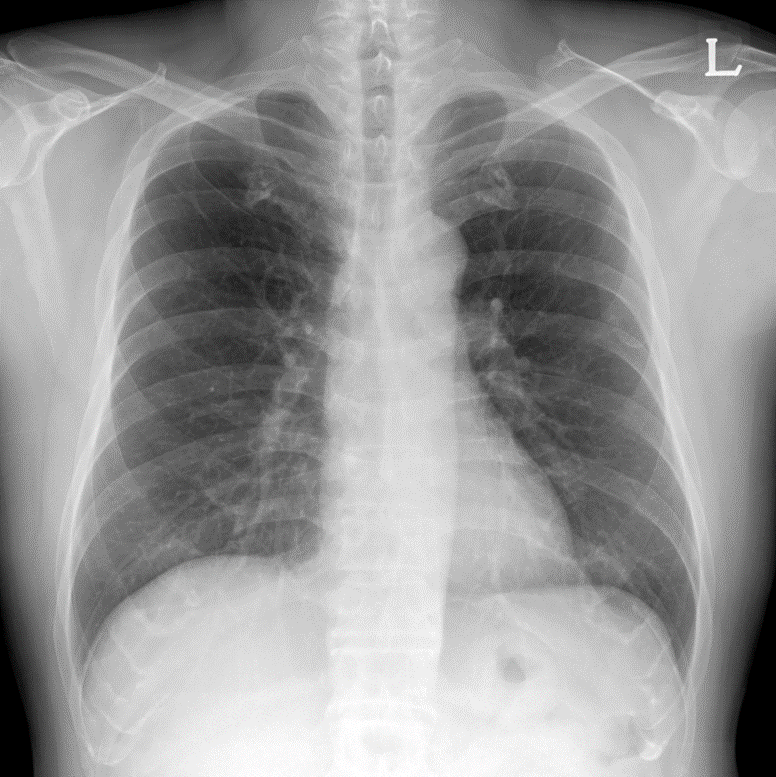
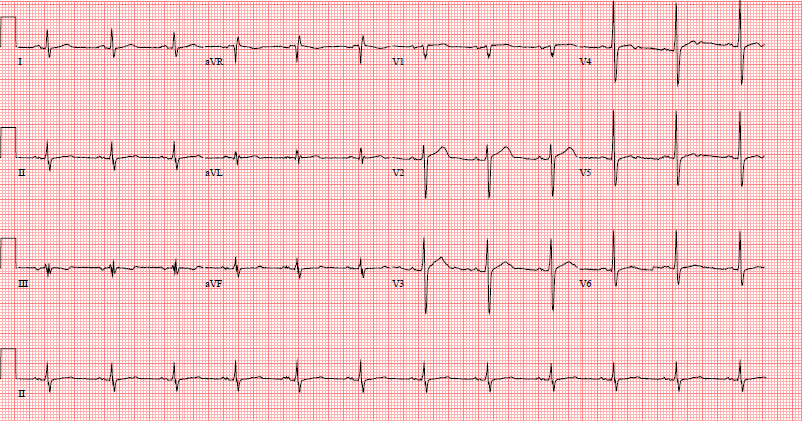
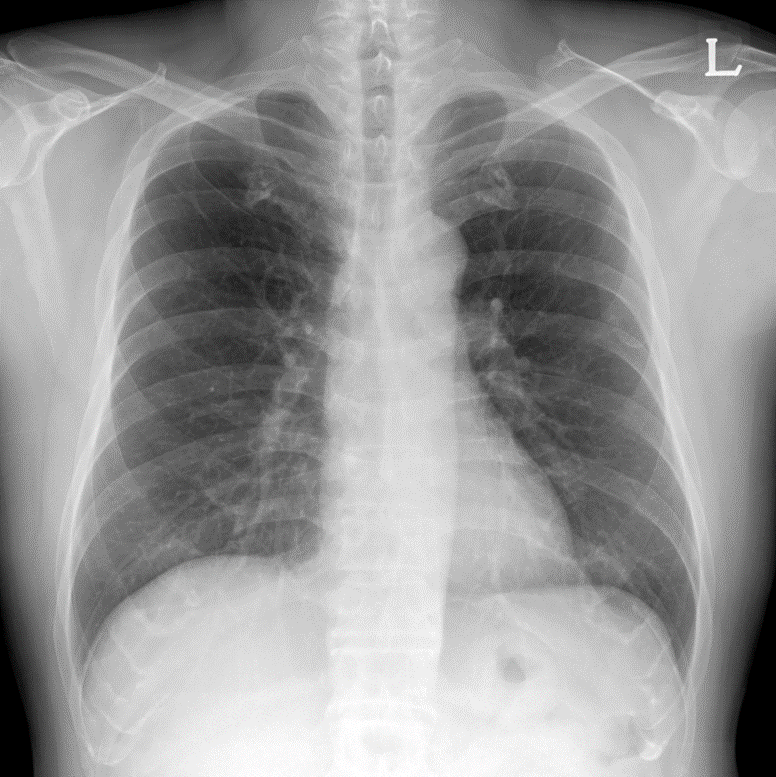
Relevant Test Results Prior to Catheterization
Echocardiography demonstrated a normal left ventricular ejection fraction but revealed akinesia of the basal septum and inferior wall. Myocardial SPECT showed a large, reversible perfusion defect in the inferior wall with an ischemia extent of 4%. Pre-procedural CT angiography identified a complex RCA CTO characterized by a severe calcified nodule at the proximal segment, predicting high difficulty for device crossing.
Relevant Catheterization Findings
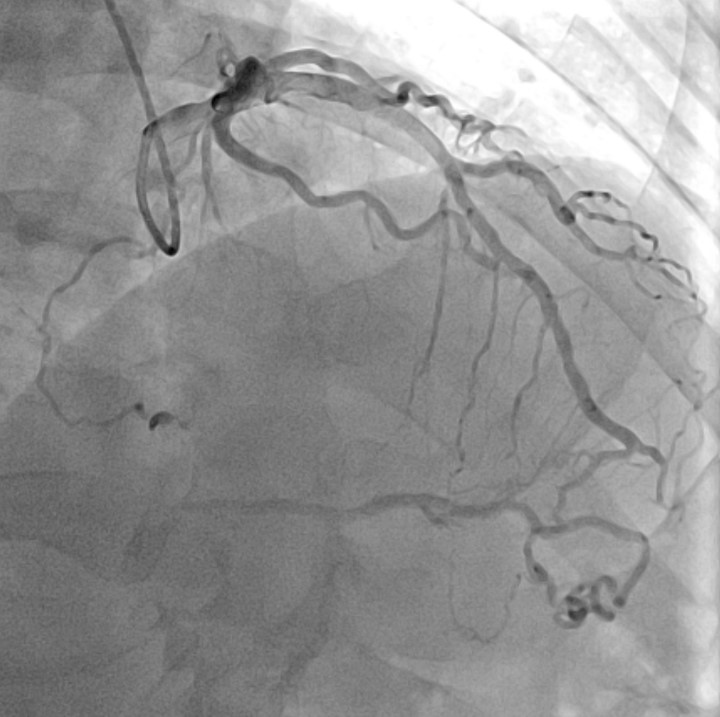
Diagnostic coronary angiography revealed a very long (>40mm) chronic total occlusion of the RCA with a J-CTO score >3. The lesion presented with ambiguous caps at both the proximal entry and distal exit points. Well-developed septal collaterals supplying the posterior descending artery (PDA) were present (CC score 3). The distal vessel architecture was further complicated by in-stent restenosis (ISR) from the previous stent implantation.


Interventional Management
Procedural Step
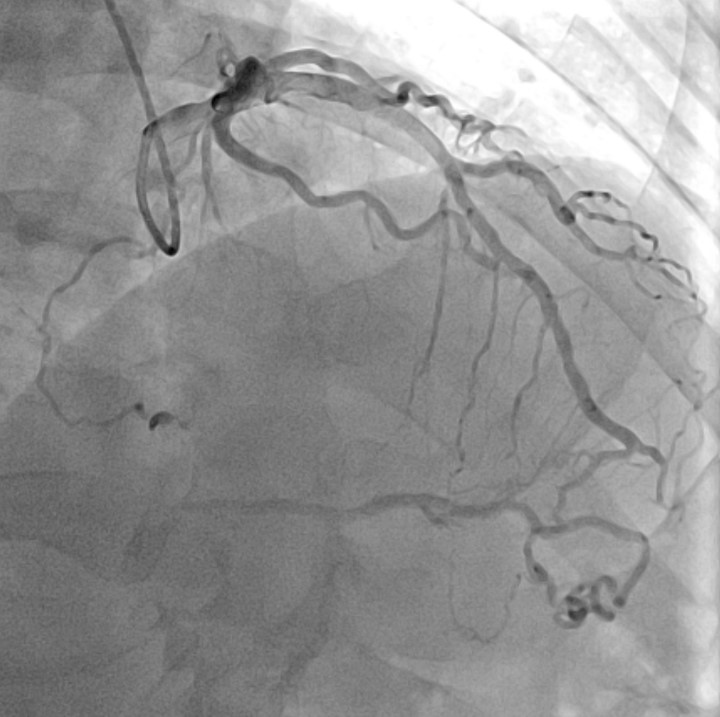
The procedure began with an antegrade attempt using a Sion wire in Corsair Pro, which failed due to the ambiguous proximal cap. We promptly switched to a retrograde approach via the septal channels. A SUOH 03 wire successfully surfed the collaterals to the distal RCA but was unable to penetrate the distal ISR segment. To bypass this barrier, we escalated to a Gladius polymer wire, which passed the ISR but tracked into the false lumen, causing a retrograde dissection. We exchanged for a Gaia Next 2 wire and carefully redirected the tip to puncture back into the true lumen near the proximal cap. Despite successful wiring, the retrograde microcatheter could not cross the calcified proximal cap to allow for externalization. To resolve this, we employed the "Tip-In" technique: an antegrade microcatheter was advanced to the tip of the retrograde wire inside the guiding catheter, and the retrograde wire was steered into the antegrade catheter to secure the rail. Following this, we exchanged for a Rota wire. Rotational Atherectomy with a 1.25mm burr was performed to modify the severe proximal calcified nodule that had prevented microcatheter passage. After IVUS-confirmed plaque modification, we implanted two overlapping Xience Skypoint stents (4.0 x 48 mm) and performed high-pressure post-dilatation with a 4.5mm non-compliant balloon.
 5_1 dual injection.mp4
5_1 dual injection.mp4
 5_2 tip in.mp4
5_2 tip in.mp4
 5_3 Final CAG.mp4
5_3 Final CAG.mp4
Case Summary
This case illustrates a comprehensive management strategy for complex RCA CTOs featuring ambiguous caps and severe calcification. It emphasizes the importance of early retrograde switching in ambiguous anatomy and demonstrates the management of retrograde dissection via wire de-escalation and re-entry. Crucially, the "Tip-In" technique is useful for failed externalization and reinforces the necessity of calcium modification using rotational atherectomy in CTO interventions.
