CASE20210812_001
Intracoronary Imaging: The Good, Bad and Ugly
By , ,
Presenter
Hashrul Rashid
Authors
1, 1, 1
Affiliation
, Australia1
Complications - Complications
Intracoronary Imaging: The Good, Bad and Ugly
1, 1, 1
, Australia1
Clinical Information
Patient initials or Identifier Number
IP
Relevant Clinical History and Physical Exam
79M presented to our Cathlab for an elective percutaneous coronary intervention (PCI) to distal LAD. He has had previous PCI to RCA, type 2 diabetes and hyperlipidaemia. He was on three anti-anginal therapy on admission to Cathlab. His examination was unremarkable and ECG revealed sinus bradycardia.
Relevant Test Results Prior to Catheterization
Full blood examination including complete blood count, renal function and liver function was normal.
He had a previous FFR to distal LAD that was significant (0.60) in the previous angiogram.
Relevant Catheterization Findings
LM: Large calibre with minor irregularities.
LAD: Moderate (±50%) proximal to mid disease with minor tortuosity followed by severe (80%) distal LAD stenosis.Ramus: Small calibre with minor irregularities.
LCx: Moderate calibre with minor irregularities.
RCA: Large calibre with patent mid RCA stent and minor irregularities.
Interventional Management
Procedural Step
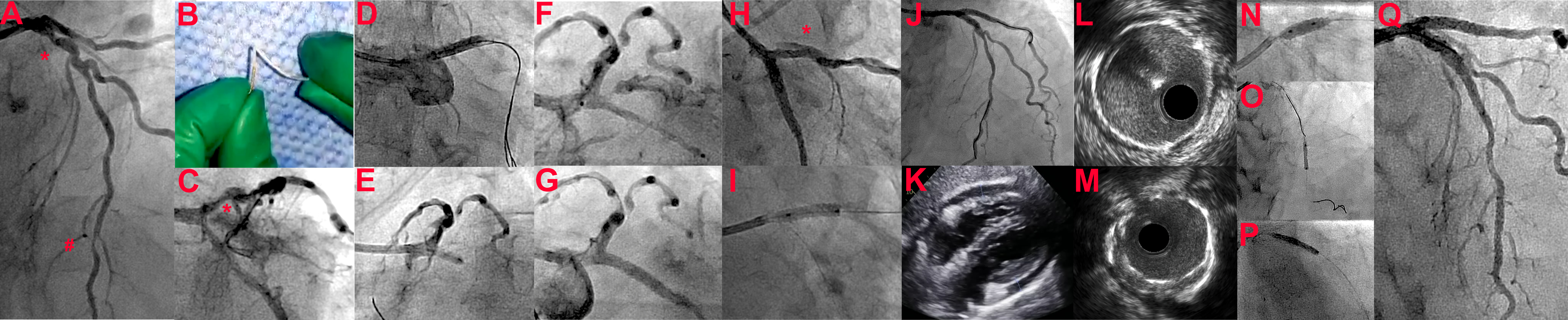
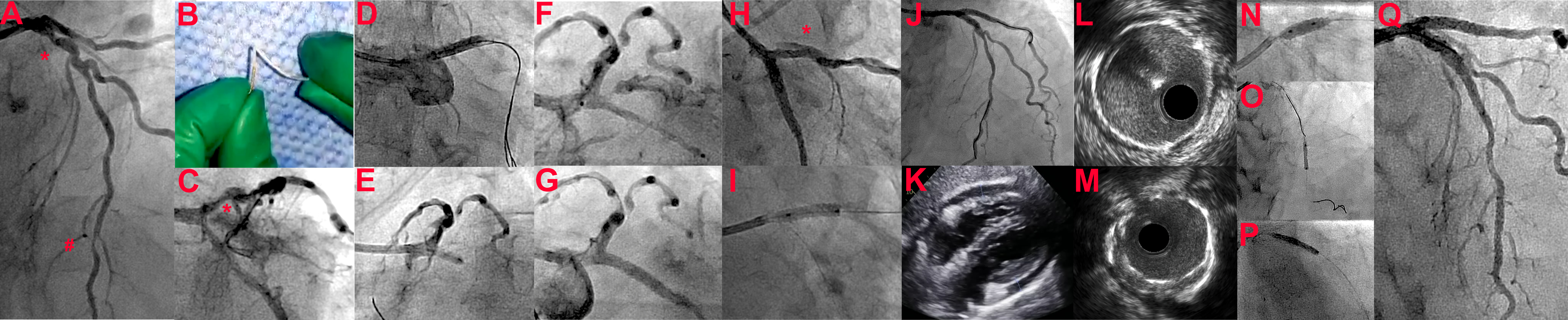
79M presented for OCT-guided PCI of (Image Panel A) severe tandem proximal (*) and distal (#) LAD stenoses for stable angina (FFR 0.62). (Image Panel B) During OCT delivery, the catheter buckled in LMCA due to LAD vessel calcification/tortuosity, (C) perforating the small calibre ramus (Type-III Ellis) (Video 1). (D) Immediate balloon inflation (3.5x12mm) at the LMCA-LAD was performed to minimise extravasation and repeated inflations facilitated LCx guidewire passage. (E) Prolonged balloon inflations (2.5x12mm) at ostial LCx were performed (15-minute intervals), but this failed to seal the perforation (Video 2). (F) A covered stent (3.0x24mm BeGraft) was deployed at the ostial LCx and post-dilated (3.5x8mm) (Video 3). (G) This sealed the perforation but there was a H) dissection(*) at proximal LAD with TIMI I flow (from initial LMCA-LAD balloon inflations) (Video 4). (I) A 3.0x12mm Xience was deployed in the LAD and this J) restored TIMI III flow. K) TTE revealed small (1cm) pericardial effusion and pericardiocentesis was averted. In a staged procedure, L) IVUS revealed optimal LCx stent implantation, but M) underexpansion of LAD stent.(N) The LAD stent was optimised (post-dilated 4.0mm) and O) distal LAD was stented (2.25x15mm Xience). FFR demonstrated Pd step-up across mid LAD (0.720.88) and P) a 2.5x18mm Xience was deployed (post-dilated 3.75mm). Q) Excellent final angiographic outcome and patient discharged after two days (Video 5).
 Video 1.mp4
Video 1.mp4
 Video 2.mp4
Video 2.mp4
 Video 3.mp4
Video 3.mp4
 Video 4.mp4
Video 4.mp4
 Video 5.mp4
Video 5.mp4
Case Summary
In summary, this gentleman had a coronary perforation of the ramus artery from a buckled OCT catheter tip, the first to our knowledge. This was treated with a covered stent to the LCx, sealing the ramus origin. He also had a Type B coronary dissection of the ostioproximal LAD, treated with a stent. In a staged procedure, he had an IVUS to the covered stent and IVUS/FFR guided PCI to the remaining LAD lesions.
1) OCT catheters can buckle and have potential to cause vessel injury,
2) Immediate balloon inflations following perforation can ‘buy time’ for operators to consider options,
3) Covered stents may be required in if extravasation continues despite balloon inflations.
