CASE20220826_012
A Challenging Case Report: Chronic Total Occlusion Intervention in a Heart Failure with Reduced Ejection Fraction Patient
By
Presenter
Yeon-Jik Choi
Authors
1
Affiliation
, Korea (Republic of)1
High-Risk Intervention (diabetes, heart failure, renal failure, shock, etc) - High-Risk Intervention
A Challenging Case Report: Chronic Total Occlusion Intervention in a Heart Failure with Reduced Ejection Fraction Patient
1
, Korea (Republic of)1
Clinical Information
Patient initials or Identifier Number
YHS
Relevant Clinical History and Physical Exam
A 45-year-old male pateint was admitted to the emergency room because of dyspnea, especially when lying down. He had a type II diabetes mellitus history and was achronic alcoholics(4-5 times a week, 2-3 bottles of soju), current smoker(45 pack-years). He also complained of abdominal distension and there were decreased lung sounds in bilateral lower lung fields when auscultation was conducted.
Relevant Test Results Prior to Catheterization
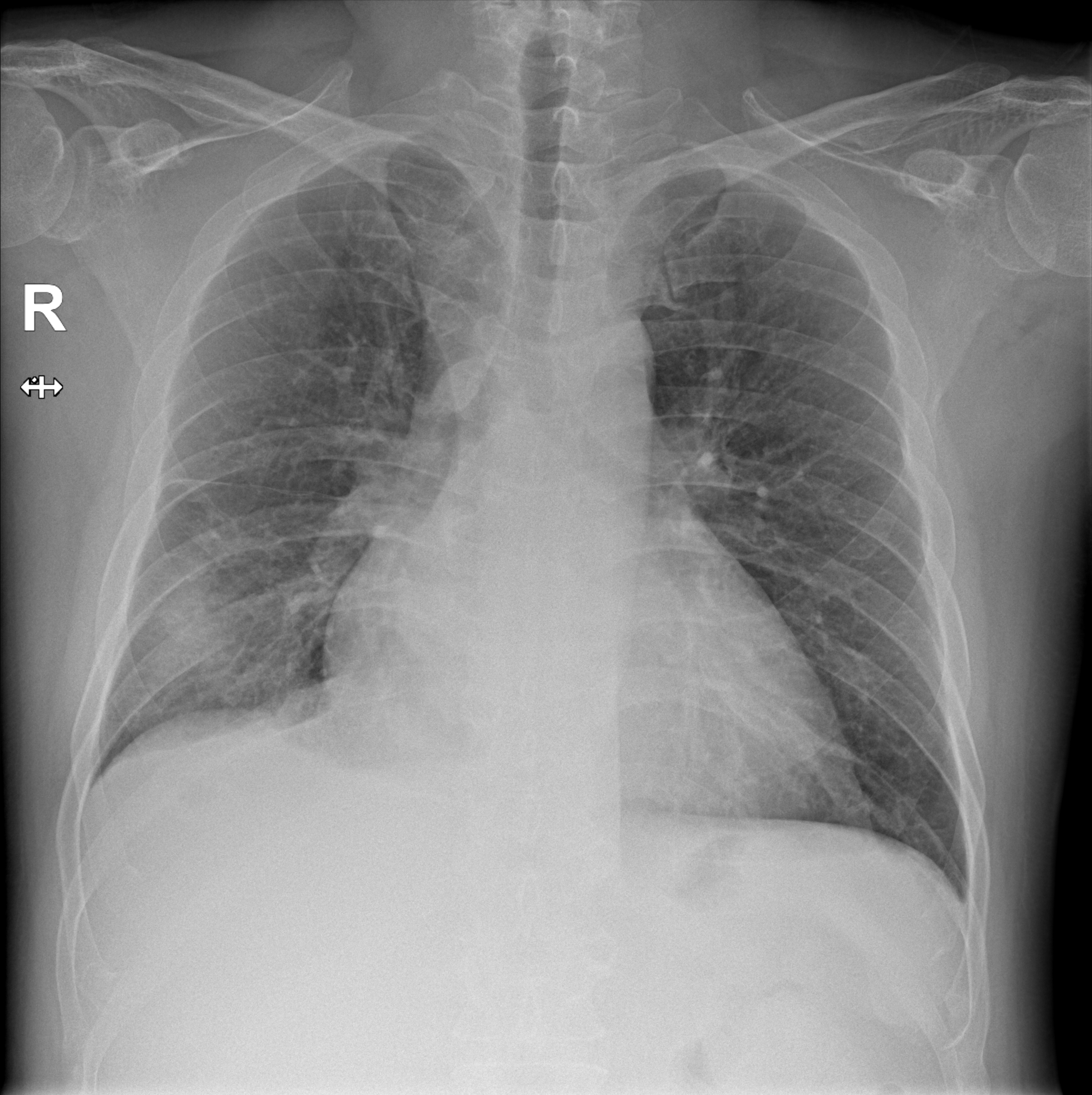
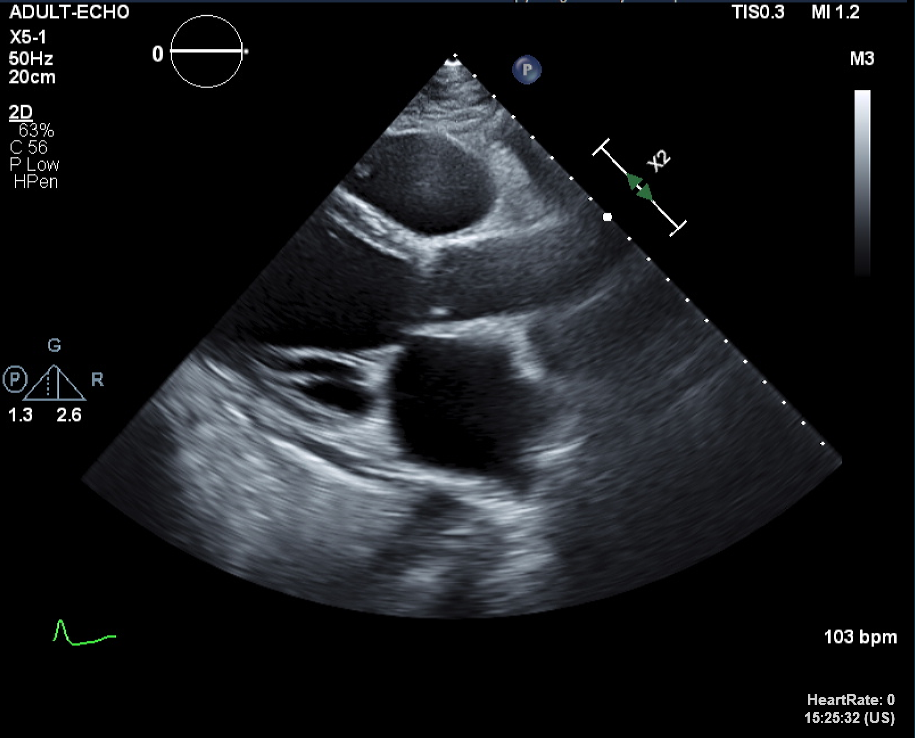
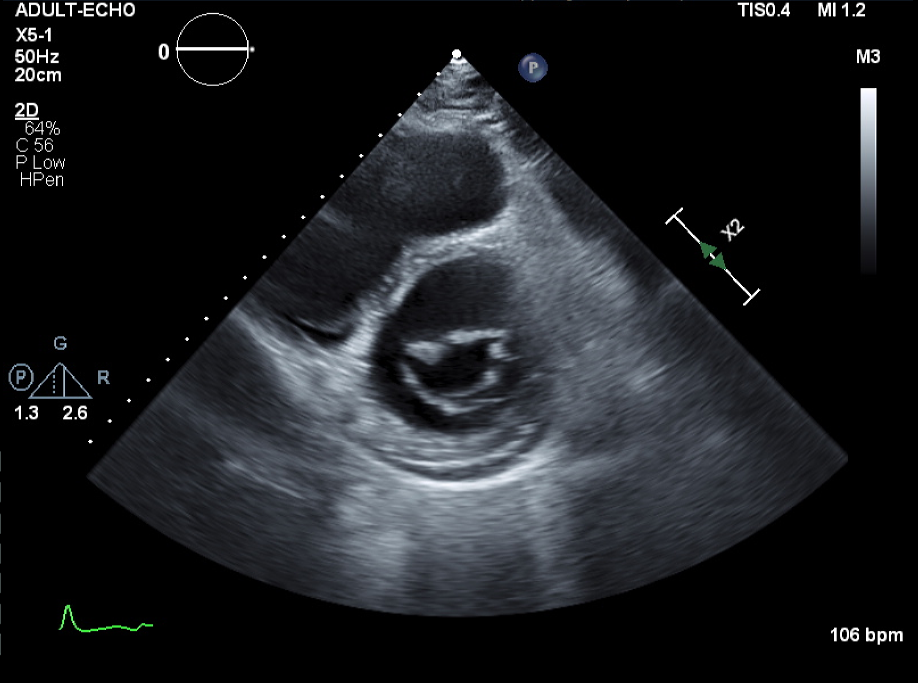
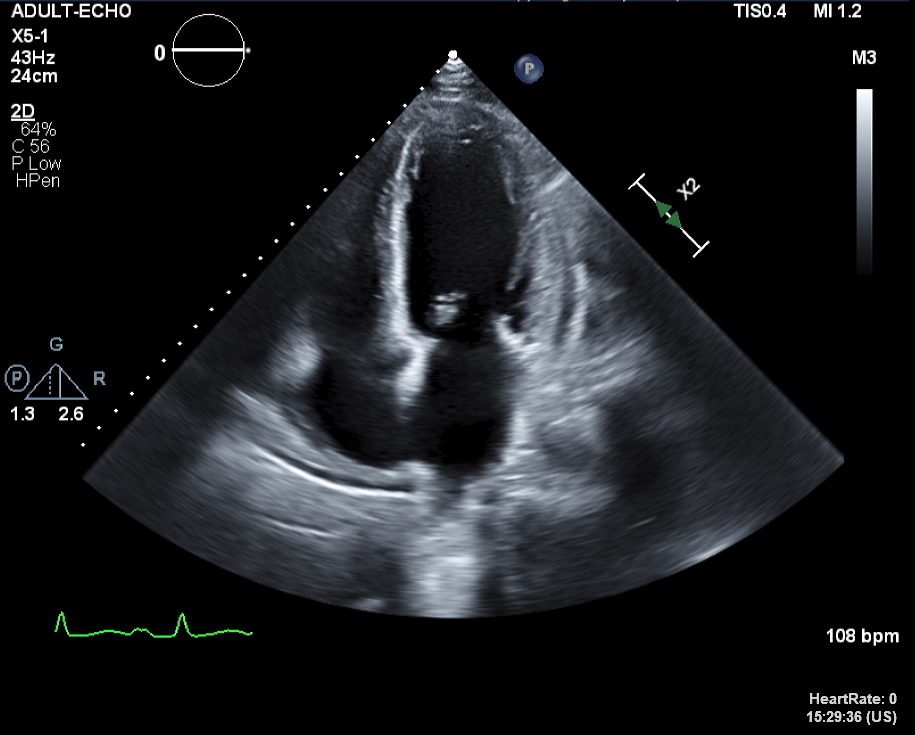
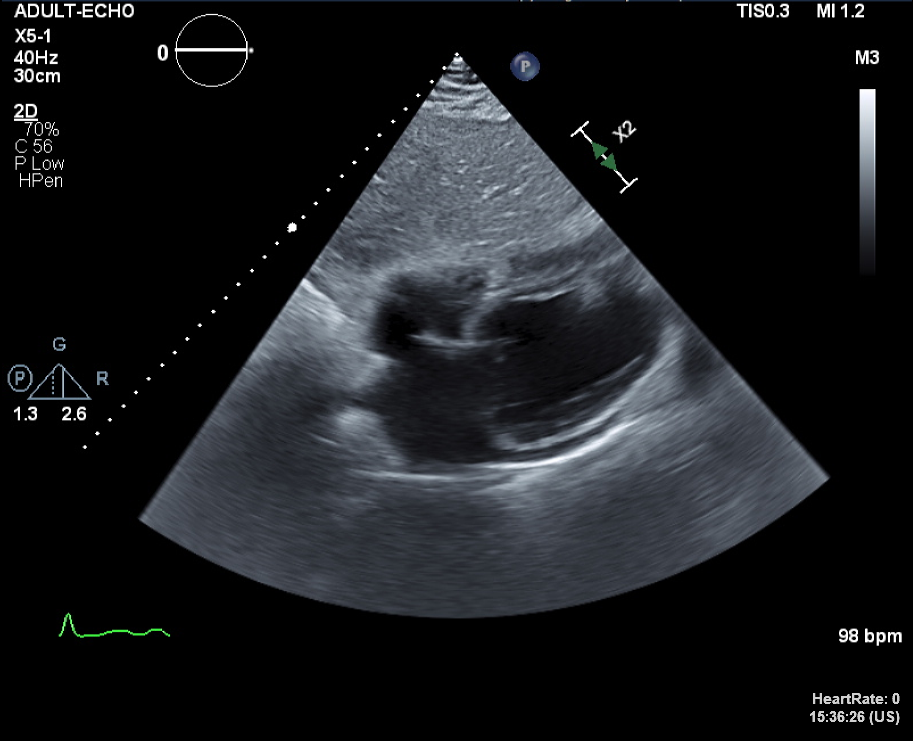
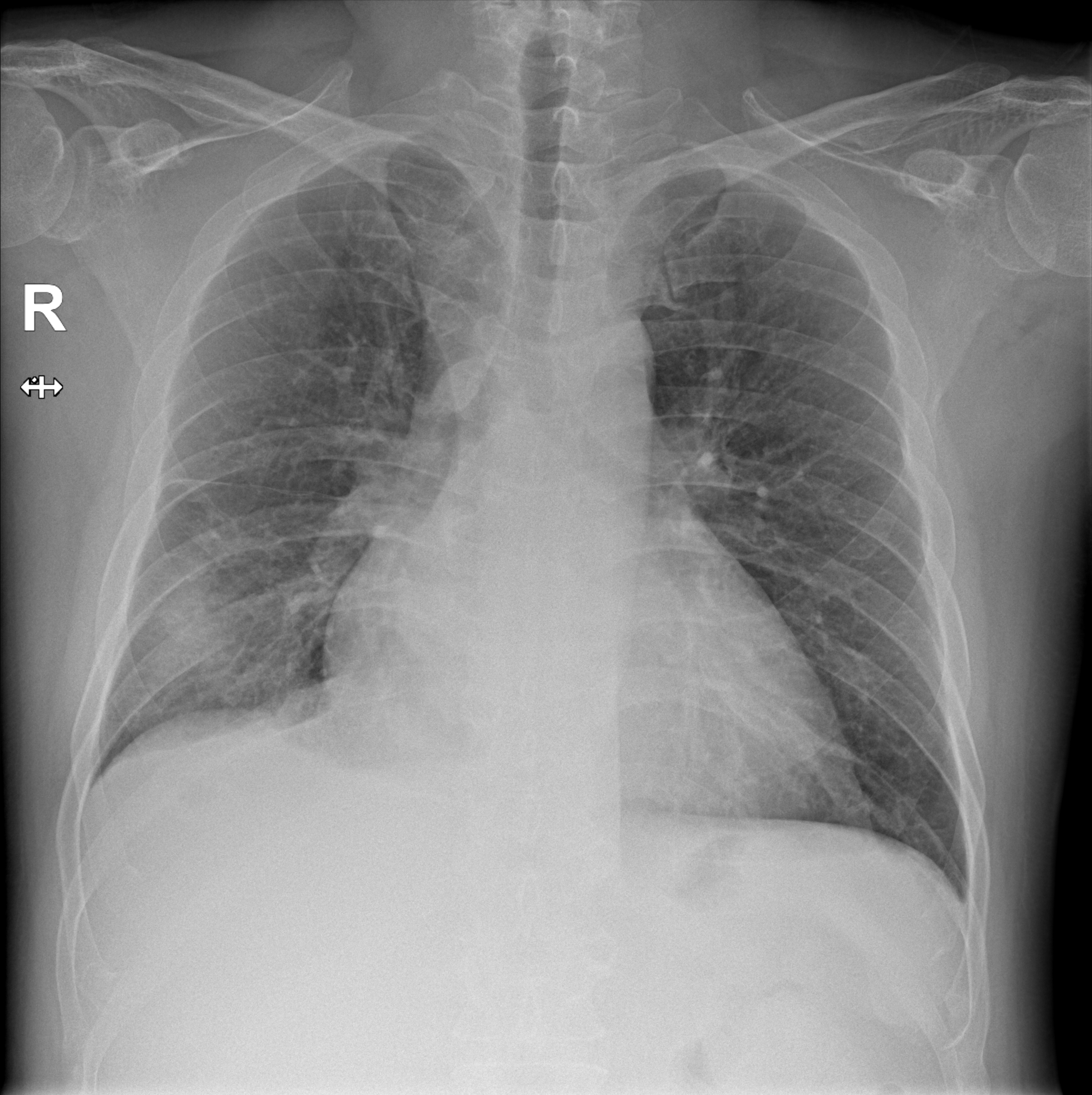
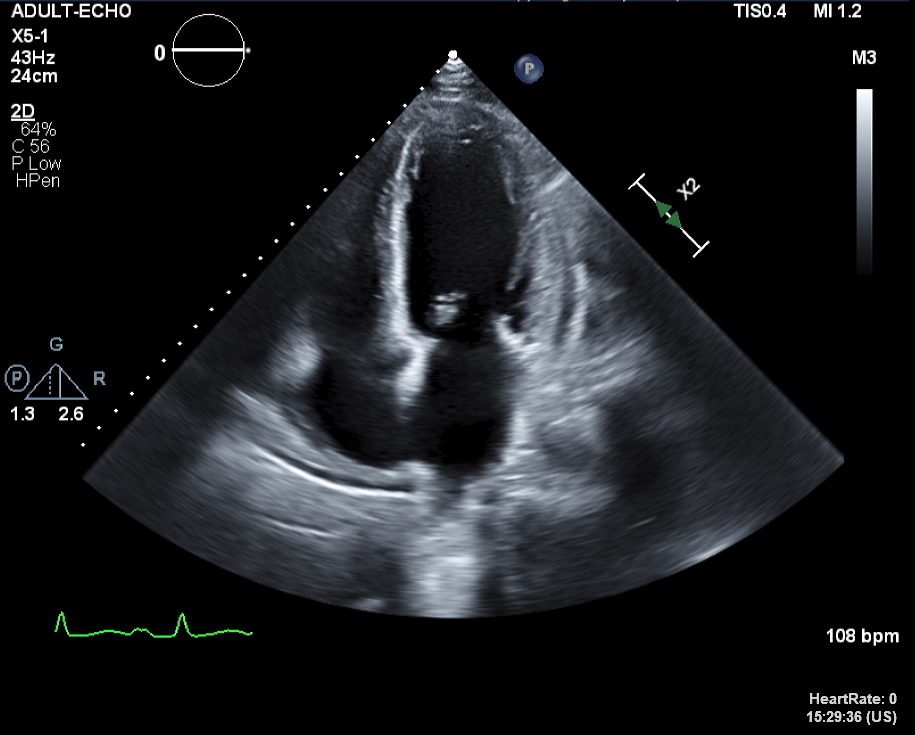
There were bilateral pleural effusion at Chest PA and Chest CT. After administration of diuretics, his symptoms were improved so, we proceeded the discharge and Transthoracic echocardiography(TTE), Thallium-201 single-photon emission computerized tomography(SPECT), 24-hours holter were conducted. In TTE, there were diffuse global hypokinesias and markedly reduced LV systolic function(LVEF=18% by biplane). Additionally, there were partially reversible ischemia in LAD/RCA territories in SPECT.
 Video 1.avi
Video 1.avi
 Video 2.wmv
Video 2.wmv
 Video 3.wmv
Video 3.wmv
 Video 4.wmv
Video 4.wmv
 Video 5.wmv
Video 5.wmv
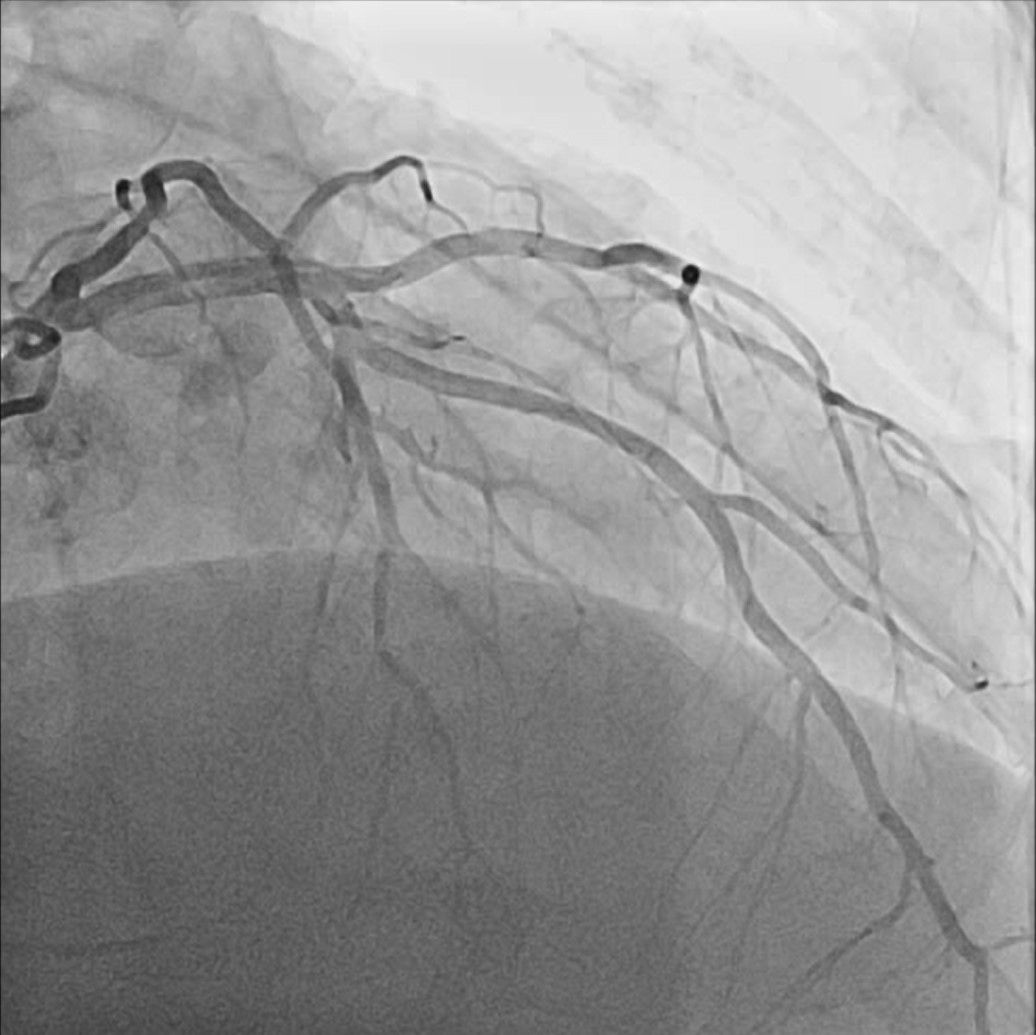
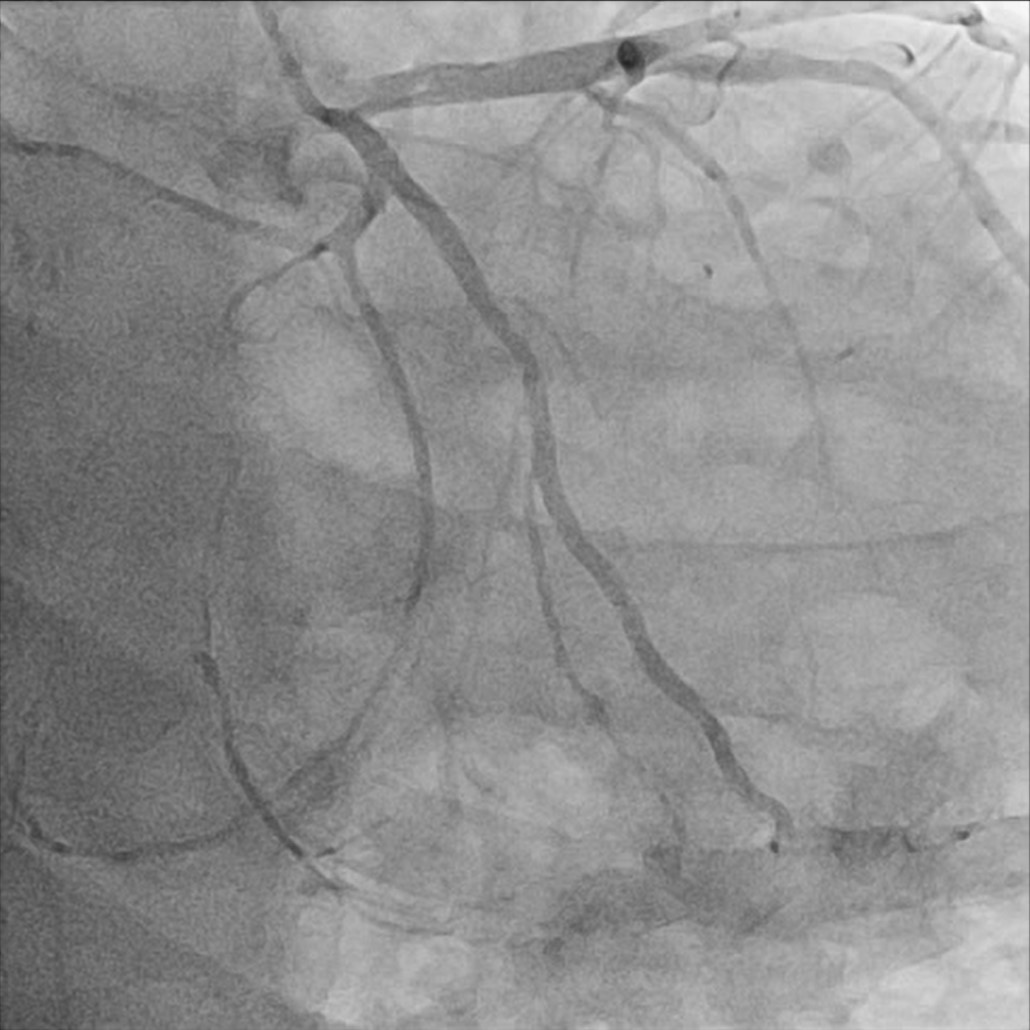
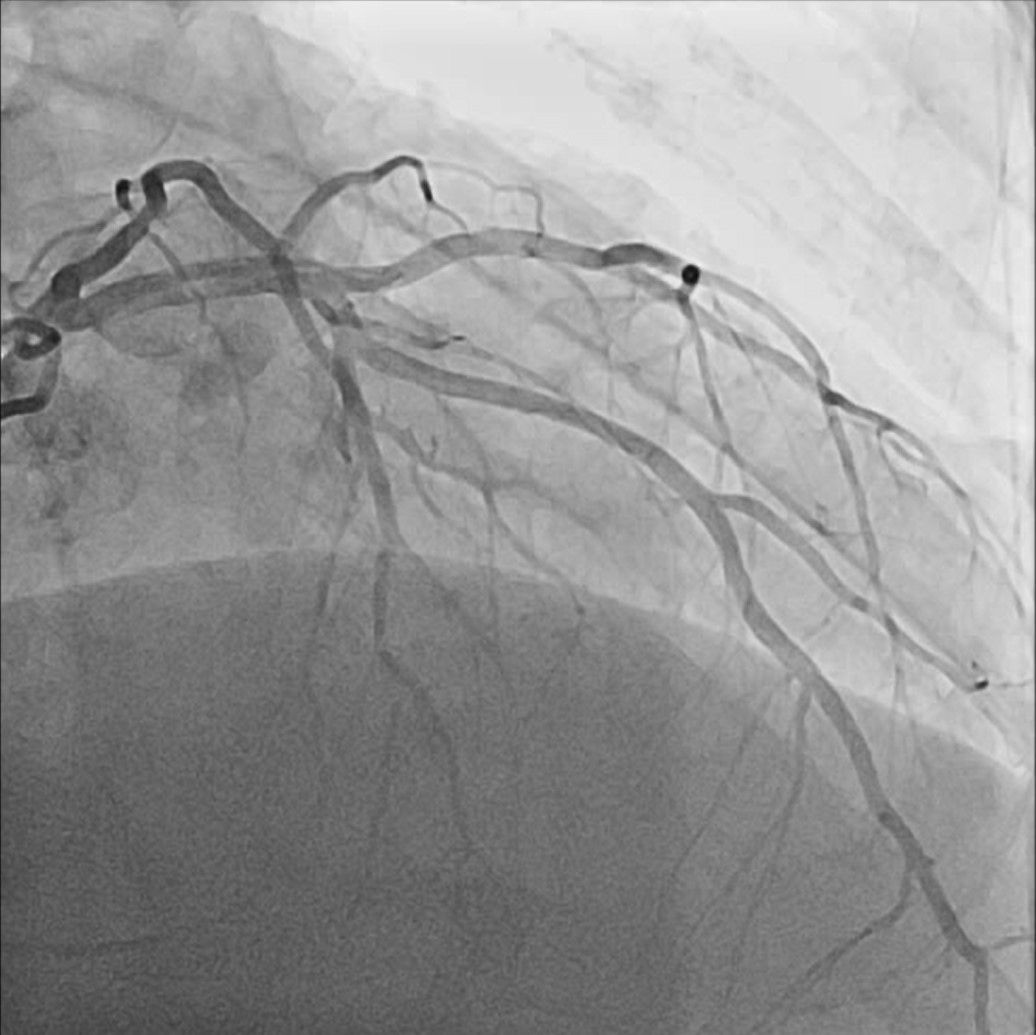
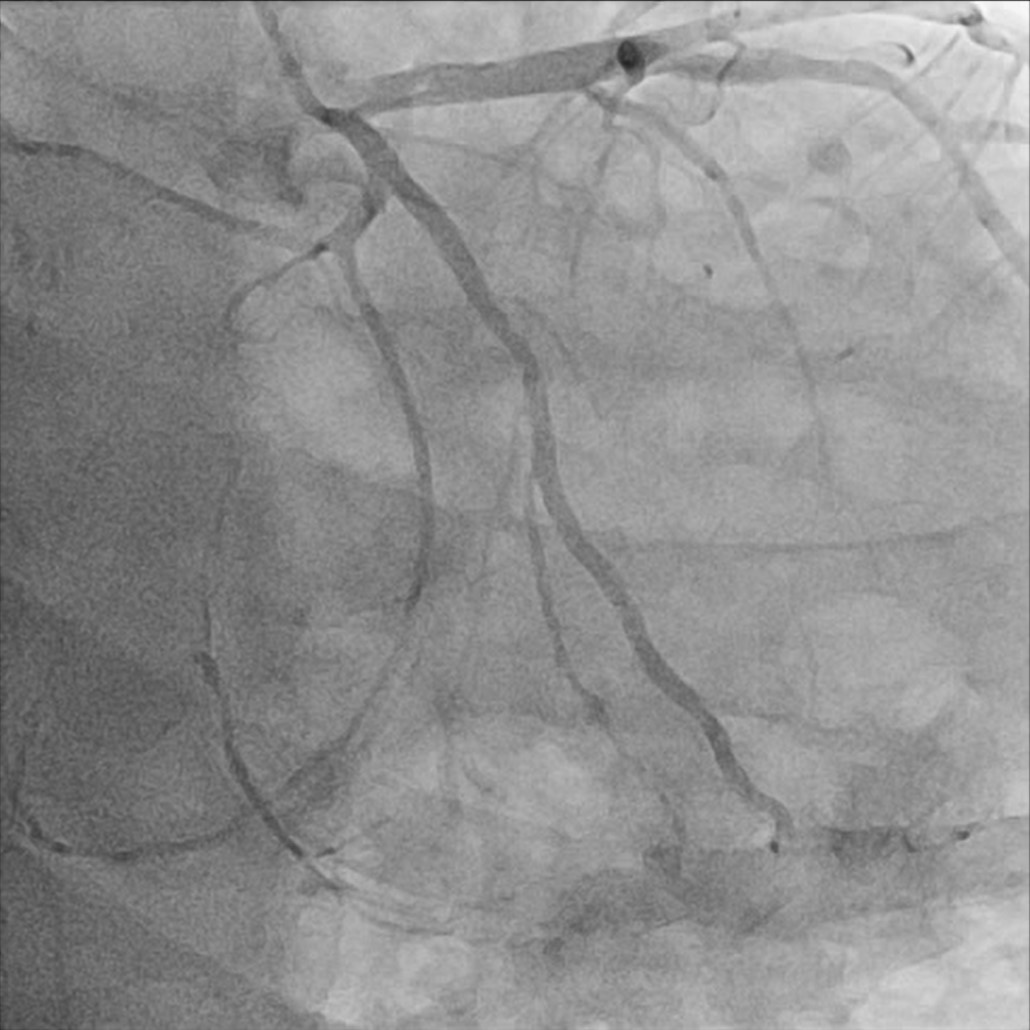
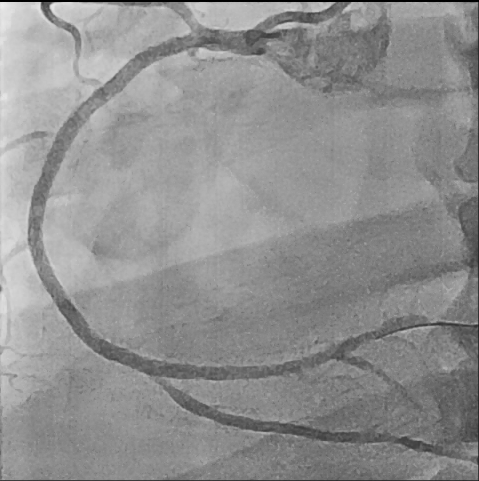
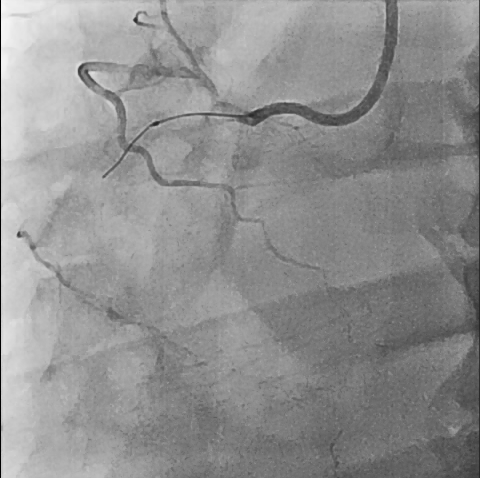
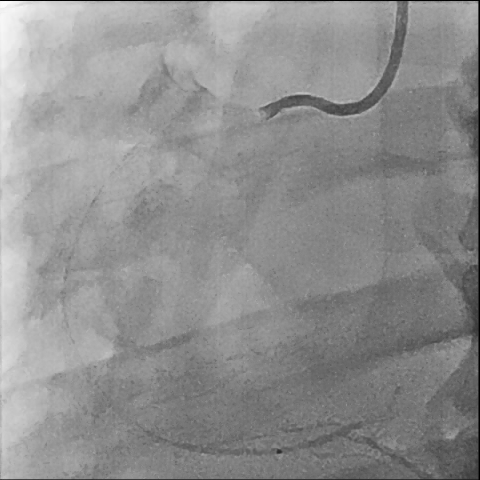
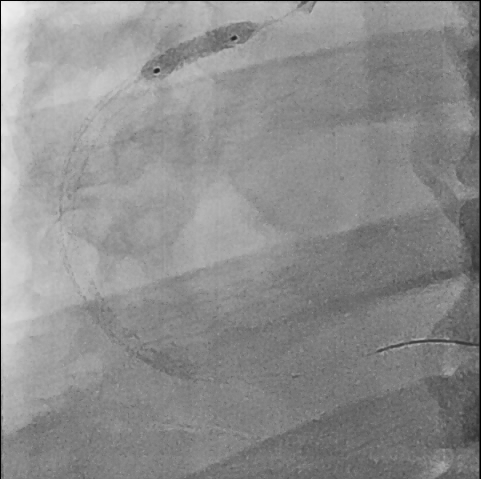
Relevant Catheterization Findings
So, we proceeded the coronary angiography. In coronary angiography, there were chronic total occlusion(CTO) of pRCA and Collateral flows from septal branch to posterior descending artery(PDA), distal left circumflex(dLCx) proper to posterolateral artery(PL). There was no significant lesion in left descending artery(LAD) and left circumflex artery(LCx). So we decided to proceed the percutaneous coronary intervention(PCI).

 Video 1.wmv
Video 1.wmv
 Video 2.wmv
Video 2.wmv
 Video 3.wmv
Video 3.wmv

Interventional Management
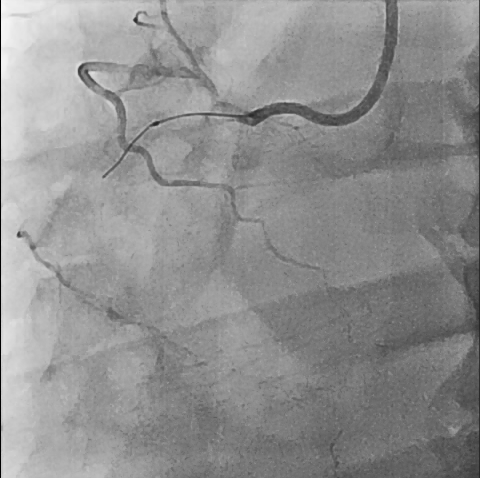
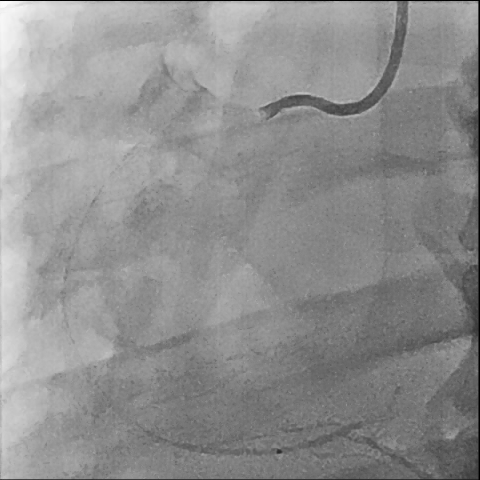
Procedural Step
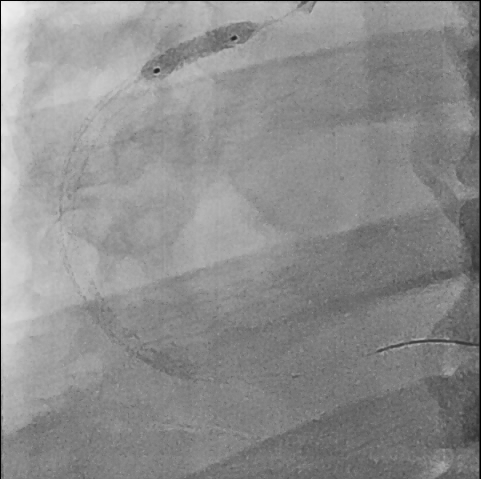
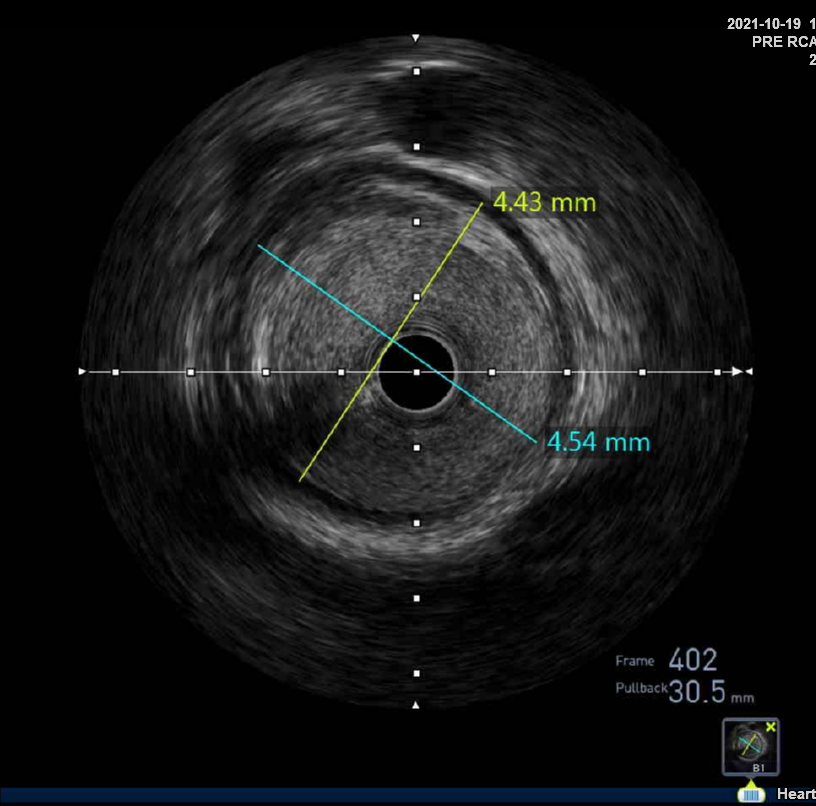
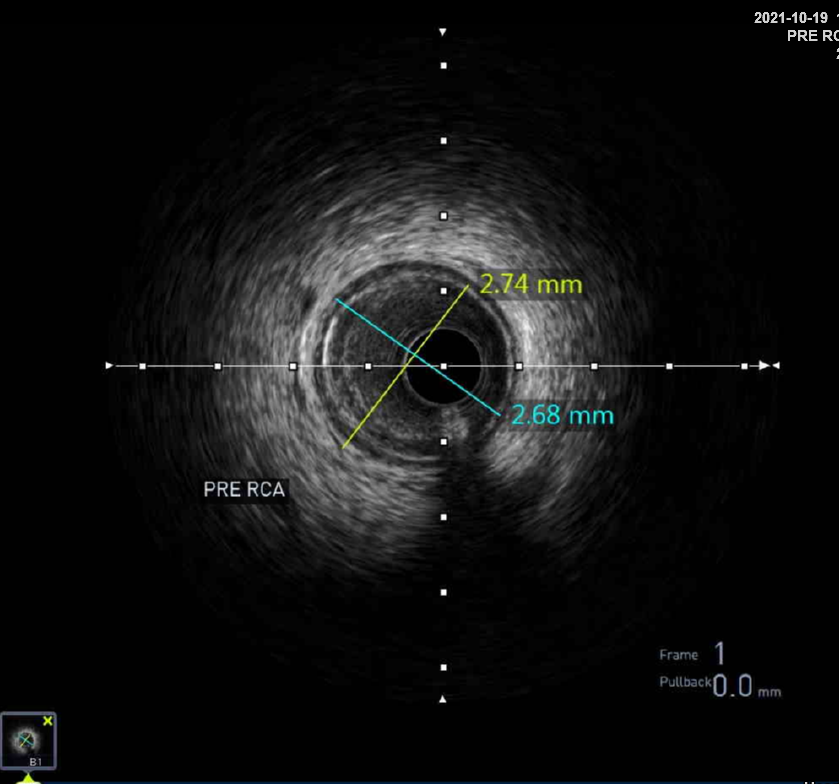
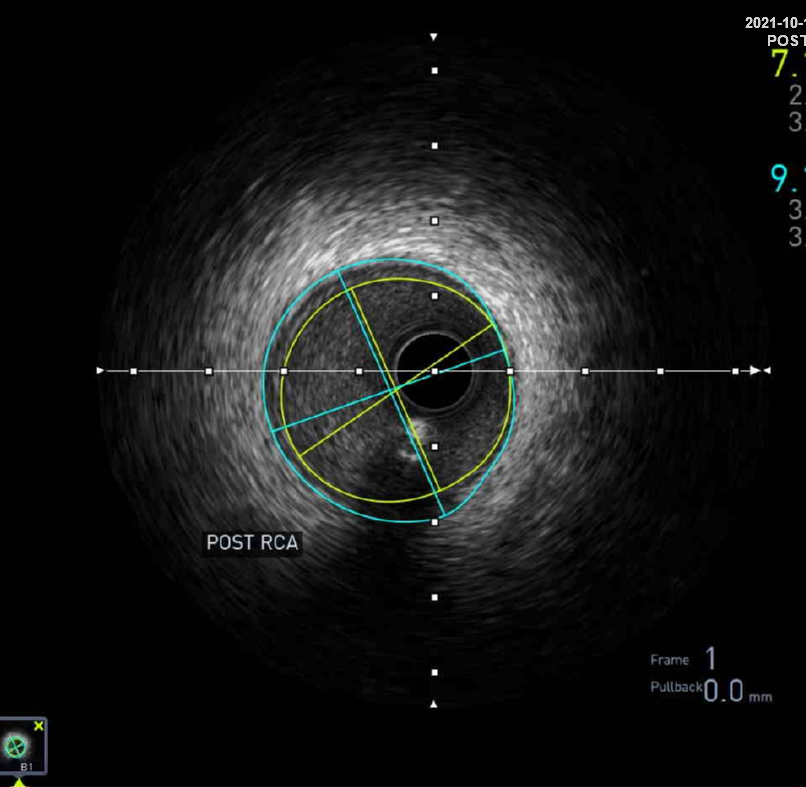
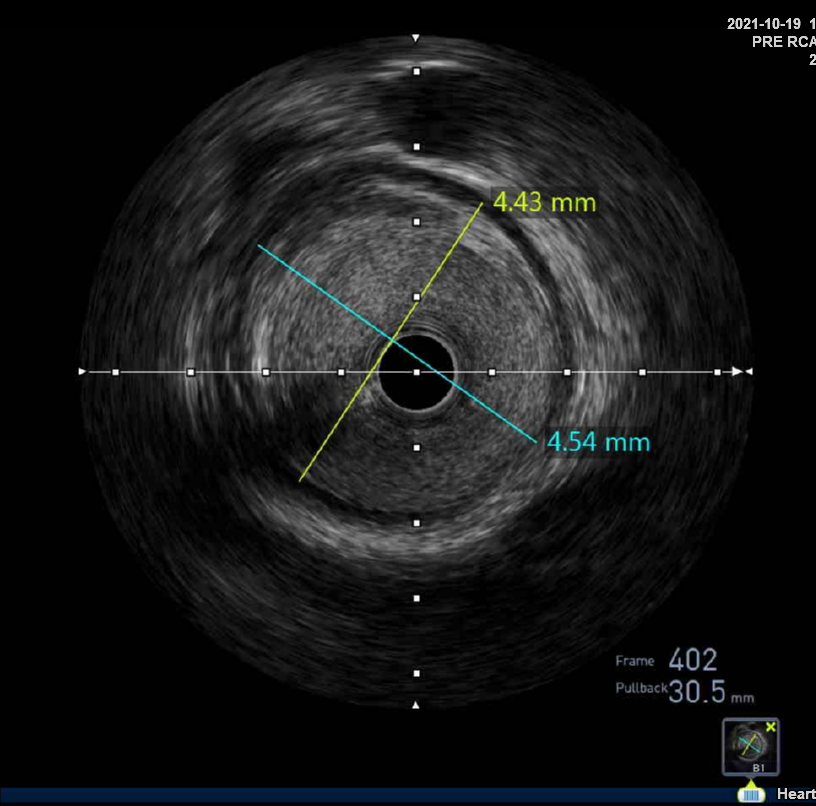
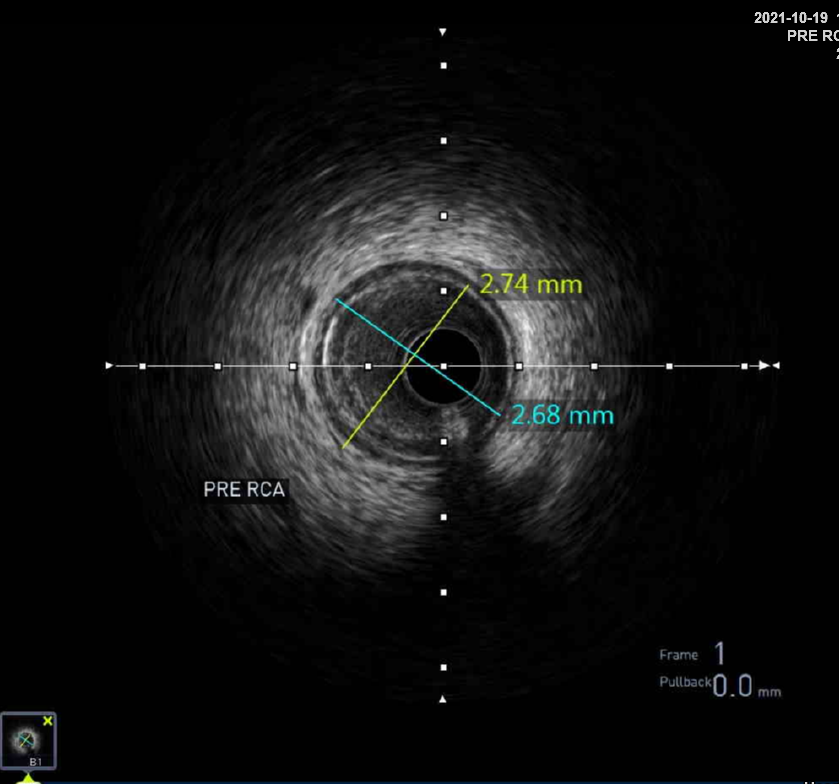
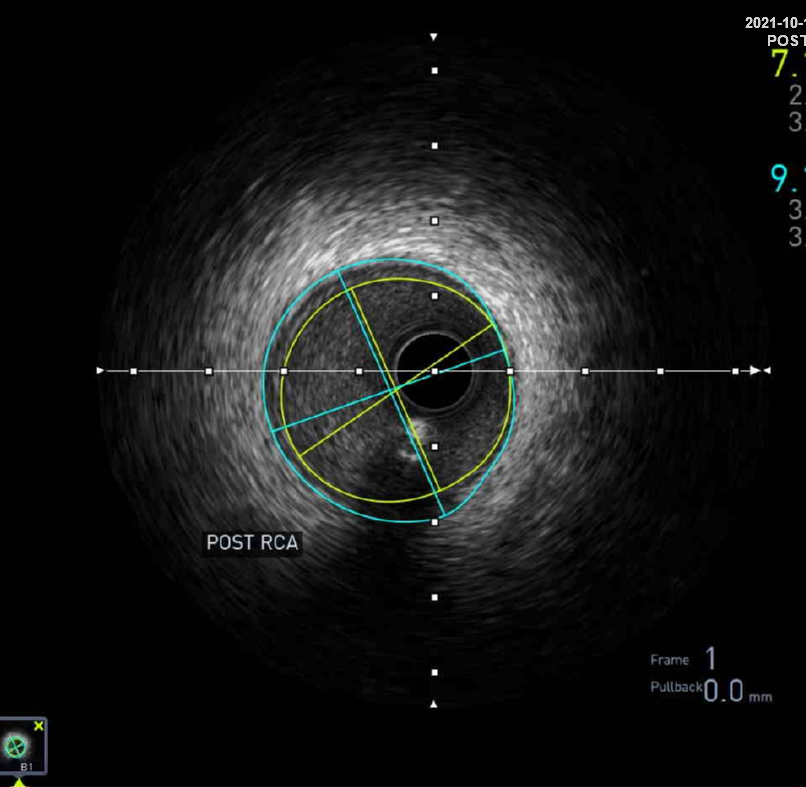
First, we did the engagement of Amplatz left(AL) guiding catheter 6-1. Then, we tried to pass the guide wire through the lesion using BMW 014" guide wire and Fielder XT-A 014" guide wire. But, we failed. So, we tried to pass the guide wire through the lesion using the Finecross microcatheter and Gaia first 014" guide wire. After we tried several times, we finally succeed to pass through the lesion. Next, Intravascular ultrasound(IVUS) was applied to examine the inside of the blood vessel in more detail. As a result, there were much burden of plaques and negative remodelling in intralumen of vessels. We tried to balloon angioplasty using selethru NC balloon 2.5*15. But, the balloon was not passed through the lesion and we had to multistage balloon angioplasty. First, we did the balloon angioplasty using Ikazuchi zero balloon 1.0*6. Then, we did the balloon angioplasty using selethru NC balloon 2.5*15. Next, the Synergy 2.75*48 drug eluting stent(DES) was inserted at mid to distal right coronary artery(RCA). Then, the Synergy 3.0*38 drug eluting stent(DES) was inserted at proximal to mid right coronary artery(RCA). Follow-up angiography and Intravascular ultrasound(IVUS) revealed that above 30% residual stenosis with stent under-expansion. So, we did adjuvant balloon angioplasty using FINE NC 3.5*15 balloon. After checking that there were no specific abnormal findings on follow-up angiography and Intravascular ultrasound(IVUS), we terminated the procedure.




 Video 1.wmv
Video 1.wmv
 Video 2.wmv
Video 2.wmv
 Video 3.wmv
Video 3.wmv
 Video 4.wmv
Video 4.wmv
 Video 5.wmv
Video 5.wmv
 Video 6.wmv
Video 6.wmv
 Video 7.wmv
Video 7.wmv
 Video 8.wmv
Video 8.wmv
 Video 9.wmv
Video 9.wmv
 Video 10.wmv
Video 10.wmv



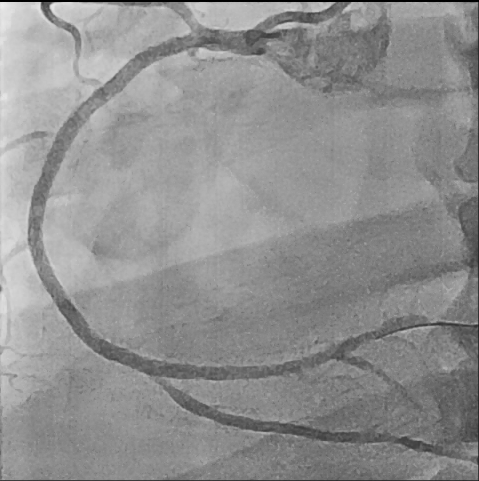

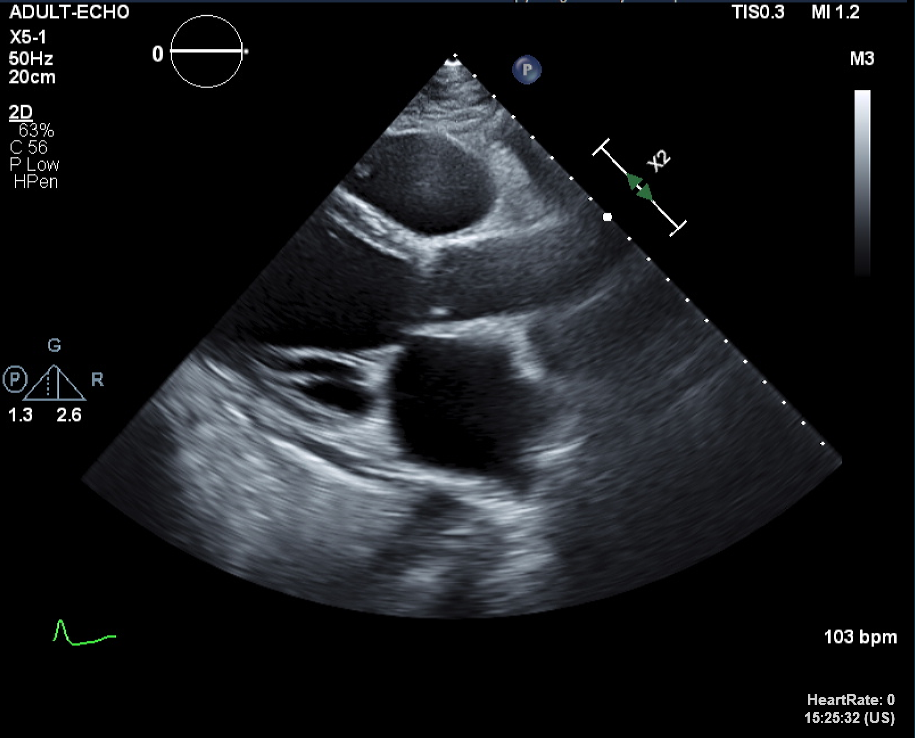
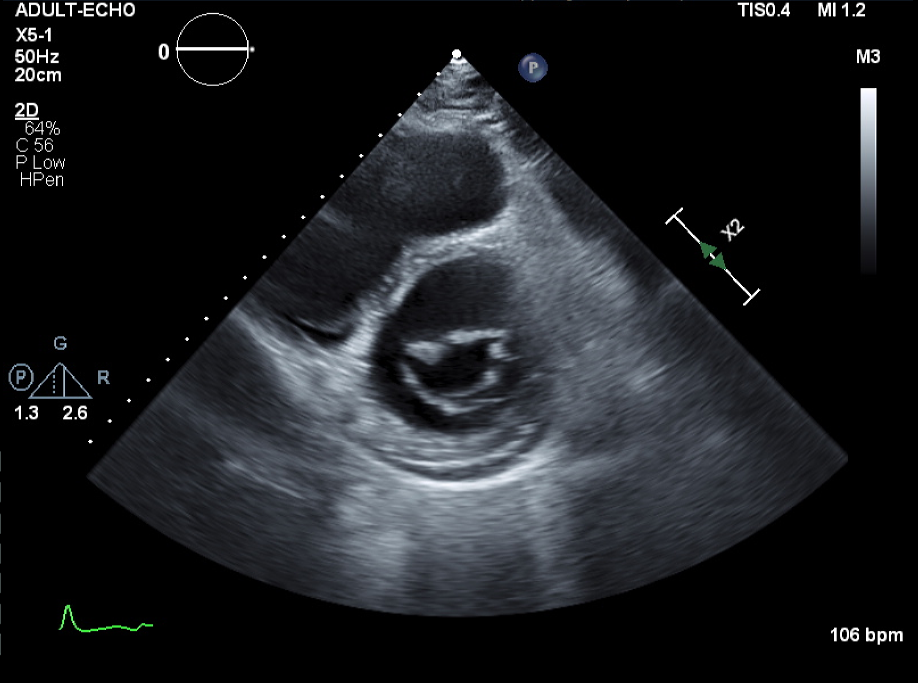
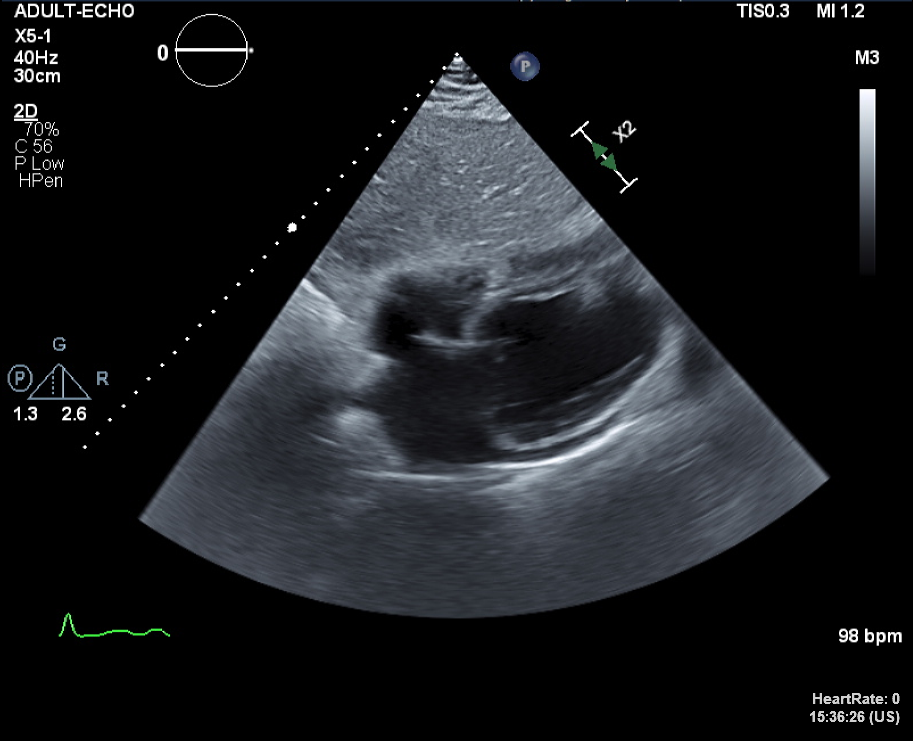
Case Summary
After intervetion, we prescribed the dual antiplatelet therapy(DAPT: aspirin 100mg, prasugrel 10mg), Statin(ezetimibe 10mg/rosuvastatin 10mg), b-blocker(carvedilol 1.5625mg bid), angiotensin receptor blocker(valsartan 40mg), diuretics(furosemide 40mg bid), mineralocorticoid receptor antagonist(spironolactone 12.5mg bid), digoxin 0.25mg. Due to insurance issues, we changed the medication from angiotensin receptor blocker(valsartan 40mg) to angiotensin receptor neprylsin inhibito(ARNI: Entresto 25mg bid). 6 months later, in follow-up TTE, his LV systolic function has been improved from 18% to 55%. This is a good case in which the heart function has improved due to successful CTO PCI and ARNI.
