Evidence ‘reconciles’ 2 apparently different revasc procedures – PCI and CABG – for LM, MVCAD
At COMPLEX PCI 2022, Gregg W. Stone, MD notes all specialists agree on choice between PCI, CABG for most patients with LM, highlights best strategies for subgroups
Recently published meta-analyses are laying the groundwork for “evidence-based reconciliation” between cardiac surgeons and interventionalists, an expert said, when determining an optimal revascularization strategy for patients with coronary artery disease (CAD).
The longstanding and tortuous contention over whether percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) surgery is the best treatment for patients with left main (LM)-CAD or multivessel (MV)-CAD has spurred several conflicting studies, both randomized and non-randomized, and heated debates over the years
Gregg W. Stone, MD (Icahn School of Medicine at Mount Sinai, New York, USA) discusses PCI and CABG as treatment options for patients with LMCAD and MVCAD at COMPLEX PCI 2022 held at the GrandWalkerhill Seoul in South Korea on Nov 25.
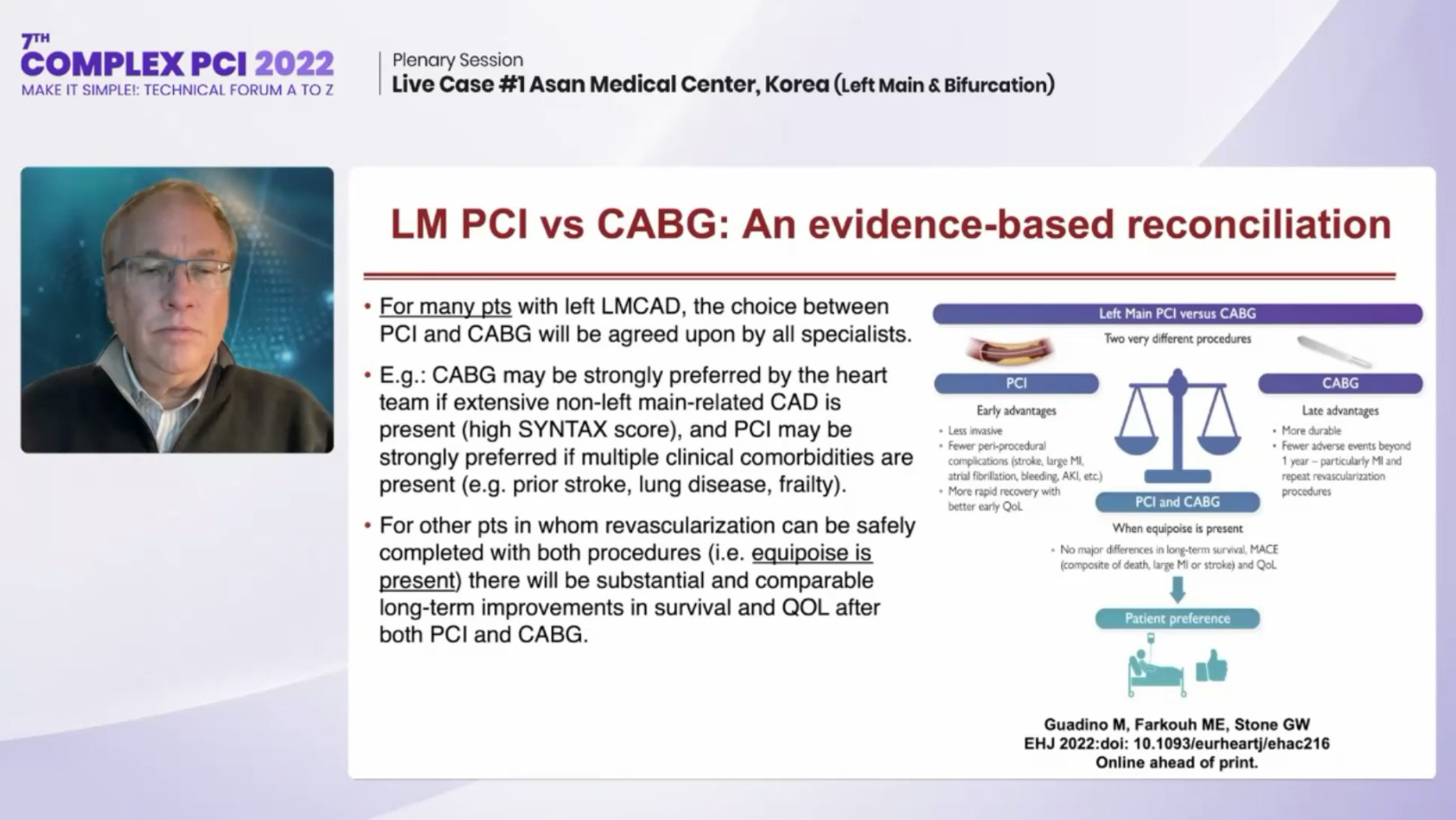
Experts are now mending the rift with conclusions of PCI and CABG being different, but complementary, procedures that produce relatively similar outcomes for the major endpoints of all-cause mortality, stroke and repeat revascularization, but each with notable tradeoffs.
 “Patients are smart, and they know the difference between the revascularization options for extensive CAD,” Gregg W. Stone, MD(Icahn School of Medicine at Mount Sinai, New York, USA) said at COMPLEX PCI 2022 held at the Grand Walkerhill Seoul in South Korea on Nov 25. “Surgery is an incredible procedure but the recovery time is not insignificant, leading to most patients preferring PCI over CABG.”
“Patients are smart, and they know the difference between the revascularization options for extensive CAD,” Gregg W. Stone, MD(Icahn School of Medicine at Mount Sinai, New York, USA) said at COMPLEX PCI 2022 held at the Grand Walkerhill Seoul in South Korea on Nov 25. “Surgery is an incredible procedure but the recovery time is not insignificant, leading to most patients preferring PCI over CABG.”
“For many patients with LMCAD, all specialists agree on the choice between PCI and CABG,” Stone said. ”CABG is often preferred for patients with extensive non-LM-related CAD and high SYNTAX scores while PCI is preferred for patients with multiple comorbidities such as prior stroke, lung disease or frailty.”
“When clinical equipoise is present and either strategy can be done safely, both PCI and CABG provide substantial and comparable long-term improvements in survival and quality-of-life (QoL),” he said. “During the decision-making process, the heart team should consider the patient’s preferences regarding the early versus late trade-offs of each strategy.”
PCI, known as the “less invasive” stenting procedure, is associated with fewer peri-procedural complications such as stroke, large myocardial infarction (MI), atrial fibrillation, bleeding and acute kidney injury, among others, compared to CABG. Studies have also shown more rapid recovery and higher QoL early on after PCI compared to surgery.
Open-heart CABG surgery is more “durable” than PCI and has advantages like a lower risk of long-term adverse events after the procedure, especially for the outcomes of MI and repeat revascularization.
The key question, Stone said, is to identify which patients benefit exceedingly with CABG to warrant a strong recommendation for surgery over PCI, since the former entails considerable physical discomfort and prolonged recovery.
Recent meta-analysis published by Marc S. Sabatine, MD (Brigham and Women's Hospital, Boston, USA) and colleagues in the Lancet last year, found no significant difference between PCI and CABG for the primary endpoint of 5-year all-cause mortality (PCI 11.2% vs. CABG 10.2%, HR 1.10, 95% CI, 0.91-1.32, p=0.33), concluding that the benefits and risks of the procedures should be weighed for each patient.
The meta-analysis, which compiled data from 4 major randomized trials on PCI with drug-eluting stents (DES) and CABG in 4,394 LMCAD patients also found no significant difference between arms for prespecified subgroups (age, sex, diabetes status, LVEF, number of diseased vessels and SYNTAX scores, among others).
A significant difference favored CABG only for “very complex” LMCAD patients with SYNTAX scores over 45, Stone said.
Regarding stroke risk – a factor that “may be more important than mortality for some” – analysis indicated a 1% absolute difference favoring CABG during the periprocedural period for up to 1-year, indicating that the risk of stroke should be weighed against the risk of mortality for LM patients.
However, the difference in stroke risk was driven by a markedly higher rate of late (>1-year) strokes in patients treated with PCI in the NOBLE trial, Stone said, especially considering none of the other 3 trials or any prior trial on PCI versus CABG showed a higher stroke risk in the LMCAD group.
For MVCAD patients, who have higher rates of diffuse, complex coronary disease than patients with LMCAD, balancing the tradeoff in mortality and stroke with patient preferences is also crucial.
Pooled analysis of individual patient data published in 2018 by Stuart J. Head, MD (Erasmus University Medical Center, Rotterdam, Netherlands) and investigators in the Lancet previously showed a higher 5-year mortality rate with PCI than CABG (2.6% absolute difference; PCI 11.5% vs. CABG 8.9%; HR 1.28; 95% CI; 1.09-1.49; P=0002) – or about 0.5% per year – although most of the difference was driven by diabetic (n=3,266) and non-diabetic (n=3,774) subgroups.
Data on MVCAD patients with diabetes that included 8 randomized trials on 7,040 patients from the original pooled analysis showed that although the diabetic subgroup had a higher risk of 5-year mortality with PCI over CABG (PCI 15.5% vs. CABG 10.0%; HR 1.48; 1.19-1.84; P=0.0004), they also had a significantly lower risk of 5-year stroke with PCI (PCI 2.6% vs. CABG 3.6%; HR 0.74; 95% CI; 0.56-0.99; P=0.039).
The non-diabetic MVCAD group had comparable rates for 5-year mortality between PCI and CABG (PCI 8.7% vs. CABG 8.0%) and 5-year stroke risk (PCI 2.6% vs. CABG 2.4%; P=0.004).
“Mortality risk should be offset with the risk of stroke, which was around 1% higher with CABG compared to PCI (3.6% vs. 2.6) for MVCAD patients with diabetes,” Stone said. “For the non-diabetic patient group, it seems like a good tradeoff; meanwhile, diabetic patients should be informed of the competing risks.”
“Discussion other outcomes – including procedural MI, non-procedural MI, dyspnea and fatigue, infections, arrhythmias, renal dysfunction, chest pain, repeat revascularization, cognitive decline, and depression, among others – could go on for hours but the bottom line is that patients want to live longer, and live better,” he said. “Anything other than mortality is encapsulated in the QoL metric that includes all non-fatal outcomes.”
2 independent sub-studies on QoL outcomes from 2017 based on the SYNTAX (n=1,800) and EXCEL (n=1,905) trials, respectively, showed no major differences between PCI and CABG.
“The SYNTAX sub-study showed no major differences in QoL and the only difference came from the Seattle Angina Questionnaire’s (SAQ) physical limitation score. Scores were much better with PCI in the first month but CABG caught up later,” Stone said. “Aside from some small differences, major late benefits were observed with both procedures.”
“The EXCEL sub-study also showed similar QoL outcomes beyond 12 months but researchers found better outcomes with PCI in the first month. Again, CABG caught up to PCI between the 1-month and 1-year period,” he added. “And this is what patients know – it takes about 6 months to recover from physical and mental changes after CABG, but both PCI and CABG are excellent for relieving angina.”
In a joint perspective article published in the European Heart Journal in April, Mario Gaudino, MD (Cornell Medicine, New York, USA), Michael E. Farkouh, MD (University of Toronto, Toronto, Canada) and Stone concluded that PCI and CABG are different procedures with unique early and late advantages.
The procedures were similar when it came to the major outcomes of long-term survival and major adverse cardiovascular events (MACE) composite of death, large MI or stroke, they said, which helps “reconcile all outcomes.”
“Studies have shown no major differences for the important outcomes of long-term survival, MACE and QoL,” Stone said. “The goal of the heart team is not to choose a procedure for the surgeon or interventionalist but to inform patients of the early versus late tradeoffs so they can choose a strategy that reflects their goals.”
Edited by

Jung-Min Ahn , MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read BiographyGaudino, Mario, et al. “Left Main Revascularization: An Evidence-Based Reconciliation.” European Heart Journal, vol. 43, no. 25, 2022, pp. 2421–2424., doi:10.1093/eurheartj/ehac216.
Stone disclosed personal lecture honorarium from Medtronic and institutional research grants from Abbott.
